During a woman's reproductive life, the menstrual cycle is a recurring process, characterized by a sophisticated chain of physiological events, directly related to fertility.
From puberty to menopause, the female reproductive system undergoes a series of important structural and functional changes that are repeated periodically every month.
The menstrual cycle therefore represents an indicator of a woman's health, therefore it is useful to understand how it works and when it differs from normal. Knowing how to calculate it and interpret the signals that the body sends, also allows you to identify which are the most fertile days when trying to have a baby or if you want to postpone a pregnancy.
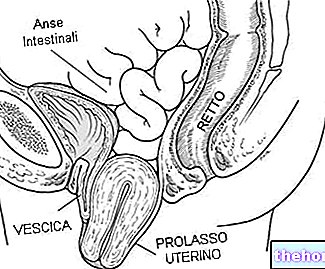
and uterus, which serve to prepare the organism for eventual fertilization and pregnancy, therefore they are fundamental for the achievement of the ultimate function of the reproductive system: the creation of a new life.
The fundamental purpose of the menstrual cycle consists, in fact, in bringing the egg cell (female gamete) to maturity and preparing an "environment" suitable for its eventual implantation. The physiological processes that follow one another during this period therefore predispose to the "beginning of a" possible pregnancy, in the event that fertilization of the oocyte occurs by a sperm of male origin.
All these processes are associated with the periodic and regular secretion of ovarian, hypothalamic and pituitary hormones, directly related to fertility. Therefore, various structures of the organism contribute to the maintenance of the menstrual cycle (central nervous system, hypothalamus, pituitary and ovaries).
(or proliferative);The beginning of each cycle is characterized by menstruation, that is, a loss of blood and tissue from the surface of the uterine wall (endometrium). During the first part of the menstrual cycle, the "endometrium changes and thickens, thus preparing to receive the cell. egg in case it is fertilized; at the same time, the oocyte undergoes processes of maturation, which end with the expulsion of the same from the ovary (ovulation). When conception does not occur, the lining of the uterine wall flakes off and is expelled with the menstrual flow; otherwise, the fertilized egg cell nestles in the uterus, where it finds the most favorable environment for its implantation and for the continuation of the pregnancy.
Duration and frequency of the Menstrual Cycle
As anticipated, the menstrual cycle is considered the period of time that goes from the 1st day of a menstruation until the day before the start of the next menstruation (note: sometimes, the actual flow is preceded by slight blood losses not yet The menstrual cycle is repeated cyclically every month, from puberty to menopause (fertile period or, more correctly, childbearing age). More precisely, the interval between the onset of two successive menstruation is generally 28 days. However, a certain variability is to be considered normal: the duration of menstrual cycles can usually range from 25 to 36 days. In these cases, the phase preceding ovulation, the so-called follicular phase (proliferative and estrogenic), may vary; on the contrary, the days that separate ovulation from the next menstruation are always 14. This second phase of the cycle is defined as luteal (secretory and progestin).
Menstruation vs Menstrual Cycle
In common parlance, the term "menstrual cycle" is often used to refer to menstruation, that is, the loss of blood that occurs every month and lasts, on average, from 3 to 7 days.
In reality:
- The MENSTRUAL CYCLE coincides with the time interval between one menstruation and the next;
- MENSTRUATIONS consist in the flaking of the mucosa that lines the inner wall of the uterus (endometrium), accompanied by a variable loss of blood through the vagina. Menstruation therefore occurs with a regular periodicity and with characteristics of fairly constant duration and quantity. .
How to calculate the duration of the Menstrual Cycle
To calculate the duration of the cycle, one must consider the period from the 1st day on which menstrual flow appears (1st day of the cycle) until the day before the start of the next menstruation.
In the case of a regular 28-day cycle, ovulation (when the ovary releases the egg cell) will occur 14 days before the next menstrual flow begins.
Regular, short and long menstrual cycles
A menstrual cycle is considered physiological when it is repeated at regular intervals of 28 days. However, a menstrual frequency of 25 to 36 days and some individual variability (the duration of the cycle can change from month to month) is to be considered normal. In any case, to be considered regular, between one menstruation and the other there must not be a "gap" of more than 4 days (more or less).
Any variations in the duration of the menstrual cycle are more likely determined by the length of the period preceding ovulation (follicular phase). This first phase of the cycle, although presenting an average duration of about 14 days, can undergo fluctuations, ranging from 1 to 3 weeks.
For most women, however, the luteal phase (period from "ovulation to" the beginning of menstruation) is more constant and takes from 12 to 16 days (average duration: 14 days).
The regularity of the menstrual cycle is related to a precise hormonal control of the phenomenon, in which the hypothalamus, pituitary and ovaries participate. The largest variations in cycle length occur in the first few years after menarche and premenopause.
). Endometrium which is conditioned - in its characteristics - by hormones such as estrogen and progesterone. These are produced by the ovary during the menstrual cycle. At the end of the cycle their production drops abruptly and - if there is no implantation - menstruation occurs.Menstruation is a sign of non-fertilization, therefore they represent the moment of lower fertility of the woman during this menstrual cycle. Typically, menstruation lasts 3-7 days, with a blood loss of about 28-80ml.
Follicular phase: preparation for ovulation
With menstruation only the upper and functional part of the endometrium is expelled, while the basal part remains which will allow a new progressive thickening of the uterine wall, which thus prepares to receive the mature egg cell if it is fertilized. Estrogens are responsible of this proliferative phase; after ovulation, the endometrium, now reconstructed, instead enters a phase of secretory maturation (regulated primarily by progesterone). This transformation is aimed precisely at the eventual implantation of the embryo.
During the first part of the menstrual cycle, - that is, from the "last menstruation to" ovulation - not only the reconstruction of the endometrium takes place, but also the growth of the so-called follicle orophore at the level of the ovary: the pituitary starts the secretion of the hormone follicle-stimulating (FSH), which stimulates the maturation of a "dominant" egg cell. Indeed, it is the follicle that produces estrogen that stimulates the proliferation of the new endometrium. For this reason the follicular phase is also called estrogenic and proliferative.
Ovulation
Around the 14th day of the cycle, a sudden increase in luteinizing hormone (LH) causes the rupture of the ovarian follicle with the expulsion of the mature oocyte inside the fallopian tube (ovulation) which, at this point, can theoretically be fertilized. During the 24 hours following this event, the egg cell is available for the eventual encounter with the spermatozoa. The release of the oocyte is therefore a fundamental prerequisite for conception.
Fertile Period
In each menstrual cycle, the fertile period, that is the most favorable moment for conception, coincides with ovulation and with the days close to this event.
If the woman has regular cycles, an oocyte (one for each menstrual cycle) takes on average 14 days to mature and, under the hormonal stimulus, to escape from the follicle that contains it to enter the tube. From here, the egg cell begins its journey towards the uterus where it nestles if, on its way, it is fertilized by a sperm.
Indicatively, the period in which it is possible for the egg to be fertilized begins 4-5 days before ovulation and ends 1-2 days later: any sexual intercourse in this fertile window can therefore lead to the onset of pregnancy. This is possible in consideration of the fact that the egg cell matures when it is expelled from the ovary can survive about 24 hours, while the spermatozoa can remain viable in the female genital system up to 72-96 hours after intercourse. window, on the other hand, conception is less likely.
The most fertile days of the menstrual cycle are identifiable by the woman herself through the detection of some characteristic signs such as those relating to the change in basal temperature or cervical mucus.
Luteal phase
Immediately after ovulation, what remains of the "burst" follicle is transformed into the corpus luteum, which produces progesterone, a hormone necessary for the early stages of a "possible pregnancy, which transforms the endometrium from proliferative to secretory (in practice , progesterone makes the uterine cavity more welcoming for the implantation of the embryo). The so-called corpus luteum is formed from the remains of the follicle that housed the oocyte, which produces progesterone.
- When conception does not take place, there is a rapid drop in progesterone levels due to the functional exhaustion of the corpus luteum. This triggers the phenomena that will lead to the flaking of the uterine wall and subsequent menstruation.
- Otherwise, the fertilized egg cell nestles in the uterus, where it finds the most favorable environment for its implantation and the continuation of the pregnancy.
For these reasons, in the absence of pregnancy, the phase that separates ovulation from subsequent menstruation is called:
- Luteinica: as the follicle is transformed into the corpus luteum.
- Progestin: Unlike the follicle which produced only estrogen, the corpus luteum also produces (and above all) progesterone.
- Secretive: since the endometrium is transformed in view of a possible nesting.
The first element of this chain is the hypothalamus, located at the base of the brain and an integral part of the central nervous system. In a nutshell, its function - in this context - is to transform nerve and electrical impulses from the brain into signals hormonal understandable by the rest of the system. In particular, the hypothalamus secretes the hormone GnRH which causes the pituitary to produce the follicle-stimulating hormone (FSH), which stimulates the maturation of a dominant follicle, containing an egg cell ( oocyte) destined to be fertilized. At the same time, the secretion of luteinizing hormone (LH) is modulated.
FSH and LH act on the ovary, the female gonad, favoring the simultaneous production of estrogen and, of course, ovulation itself; the increasing levels of estrogen in the body cause thickening of the uterine wall, through the accumulation of blood and nutrients (in this way, the fertilized egg will have the necessary support for its growth). Around the middle of the cycle, when maturation is complete, estradiol and luteinizing hormone (LH) stimulate rupture of the follicle and the egg is released into the fallopian tube, through which it travels to the uterus. Hormone levels reached by estrogen and progesterone, in turn, influence the whole upstream cascade, stimulating or inhibiting the pituitary gland to release more FSH and LH.