Chlordiazepoxide was the first benzodiazepine to enter the market in the "early 1960s". Later, changes were made to the structure of chlordiazepoxide in an attempt to obtain drugs with better characteristics. In 1959 diazepam was synthesized, a benzodiazepine up to 3-10 times more powerful than chlordiazepoxide. Diazepam was marketed in 1963 under the trade name - still used and well known today - of Valium®.
Subsequently, benzodiazepine research continued to develop, resulting in numerous new molecules that are still used today.

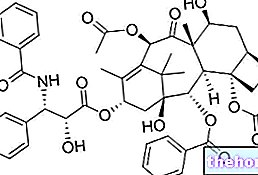
General Structure of Benzodiazepines
short term;Furthermore, benzodiazepines can be used as sedatives before exploratory examinations or treatments (gastroscopy, colonoscopy, etc.); they are also used in anesthetic premedication.
of the drug;Lipophilicity is a fundamental parameter.In fact, to carry out their action, benzodiazepines must reach the brain neurons and - to do so - they must overcome the blood brain barrier (a complex physiological system that regulates the exchange of useful substances and waste products between blood, cerebrospinal fluid and brain). One of the fundamental characteristics that any drug must possess in order to cross this barrier is, in fact, lipophilicity.
The greater the lipophilicity of a benzodiazepine, the greater the speed with which it crosses the blood brain barrier.
These factors, therefore, help determine what the clinical uses of each benzodiazepine are. For example, a rapidly absorbed benzodiazepine, whose metabolism does not generate active metabolites and is highly lipophilic, will be more useful as a hypnotic sedative, but less useful for the treatment of anxiety.
Conversely, a benzodiazepine with a slower rate of absorption and whose metabolism generates active metabolites is likely to be more useful for the treatment of anxiety states.
Deepening: How to fight anxiety?
The use of benzodiazepines - which in any case must be prescribed by the doctor - is not the only way to treat anxiety.
In fact, in the presence of anxious pathologies, it is first of all fundamental to contact the doctor and specialist for an accurate diagnosis in order to establish which disorder affects the patient, its degree of severity and its cause. From here it will then be possible to develop a therapeutic strategy that can lead to the resolution of the problem.
PLEASE NOTE: benzodiazepines must NOT be taken by the patient on his own initiative, but must be used only and exclusively if prescribed by the doctor.
it is influenced by numerous substances responsible for the exchange of information between anatomical structures that are distant from each other. The transmission of impulses is entrusted to particular messengers - neurotransmitters - which can exert an excitatory or inhibitory action.
Thanks to the role played by neurotransmitters, the organism is able to modulate its motor, sensory and intellectual activities and activities related to the affective sphere and to the tone of mood.
Benzodiazepines act by stimulating the GABAergic system, that is the "γ-aminobuttyric acid (or GABA).
GABA is a γ-amino acid and is the main inhibitory neurotransmitter in the brain. It carries out its biological functions by binding to its specific receptors: GABA-A, GABA-B and GABA-C. A benzodiazepine specific binding site (BZR) is present on the GABA-A receptor. Benzodiazepines bind to this specific site, activate the receptor and promote the inhibitory signal cascade induced by GABA itself.
See also: How do Benzodiazepines work?
(a parameter that provides information on the duration of action of each benzodiazepine):- Short or very short half-life (2-6 hours), triazolam and midazolam belong to this category;
- Intermediate half-life (6-24 hours), oxazepam, lorazepam, lormetazepam, alprazolam and temazepam belong to this category;
- Long half-life (1-4 days), this category includes chlordiazepoxide, clorazepate, diazepam, flurazepam, nitrazepam, flunitrazepam, clonazepam, prazepam and bromazepam.
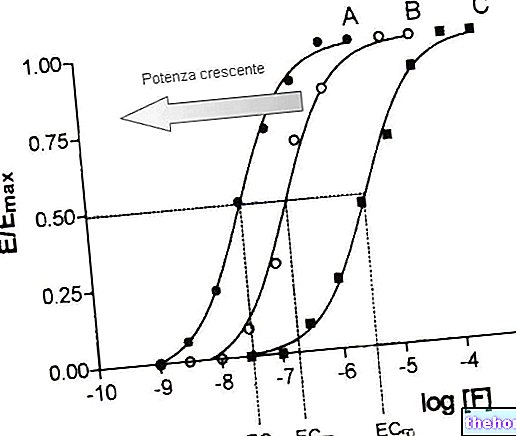
Contrary to what one might think, there is no direct relationship between plasma half-life and rapidity of action, as some drugs - while acting rapidly - are metabolized into other active compounds which significantly prolong their duration of action. A striking example is that of midazolam.
Midazolam is a benzodiazepine used as a general anesthetic to induce drowsiness or maintain sleep. It is a hydrophilic molecule, which makes it suitable for intravenous administration. However, after administration, midazolam undergoes structural changes that make it highly lipophilic, therefore capable of rapidly overcoming the blood brain barrier.
relatively low. Furthermore, they have a high therapeutic index. This parameter expresses the relationship between toxic dose and therapeutic dose.If a drug has a high therapeutic index, it means that there is a significant difference between the commonly used therapeutic dosages and the toxic dosages.
Rarely, a benzodiazepine overdose can be fatal, unless other drugs or substances capable of depressing the central nervous system, such as barbiturates, opioid drugs, alcohol or drugs, have been taken at the same time.
In any case, benzodiazepines are certainly not without side effects. Among these effects, we remember:
- Excessive sedation;
- Daytime sleepiness;
- Confusion, especially in elderly patients;
- Depression;
- Disorders of coordination;
- Ataxia;
- Memory disturbances (anterograde amnesia).
Other side effects that can occur following the intake of benzodiazepines are the so-called paradoxical symptoms.
- Restlessness;
- Agitation;
- Irritability;
- Aggression;
- Anger;
- Anger;
- Psychosis;
- Delusions;
- Hallucinations;
- Nightmares
- Disappointment;
- Behavioral changes.
It should also be remembered that benzodiazepines are susceptible to abuse and give physical and psychological dependence. Once physical dependence has established itself - following abrupt discontinuation of treatment - withdrawal symptoms may arise, such as:
- Depression;
- Derealization;
- Depersonalization;
- Anxiety;
- Confusion;
- Nervousness;
- Restlessness;
- Irritability;
- Hallucinations;
- Epileptic seizures;
- Rebound insomnia;
- Changes in mood;
- Sweating;
- Diarrhea;
- Headache
- Muscle aches;
- Hypersensitivity and intolerance to sounds (hyperacusis);
- Hypersensitivity to light and physical contact.
Therefore, gradual discontinuation of therapy is always recommended.
Abrupt interruption of therapy must also be avoided because it can cause rebound insomnia or anxiety. That is, the symptoms that induced the use of the drug (insomnia or anxiety, in fact) may recur in an aggravated manner at the end of the therapy itself.
Finally, with prolonged use of benzodiazepines, tolerance can develop. In other words, a reduction in the effects induced by the drug can be encountered, so it is necessary to take increasingly higher doses to obtain the desired effect again.
- especially during the first trimester - due to the malformations that can arise in the fetus. Furthermore, since benzodiazepines are excreted in breast milk - in most cases - their use is also contraindicated during breastfeeding.
The use of benzodiazepines is also contraindicated in the following cases:
- In patients with myasthenia gravis (a neuromuscular disease);
- In patients with severe respiratory insufficiency, as benzodiazepines can cause respiratory depression;
- In patients with severe hepatic insufficiency;
- In patients with sleep apnea syndrome;
- In patients with acute alcohol or hypnotic, analgesic, antidepressant or antipsychotic drug intoxication.