Symptoms and Complications
Symptoms of xeroderma pigmentosum concern:
- The skin, especially the parts exposed to the sun
- The eyes
- The nervous system
Since this is a congenital disease, the first signs of the disease begin to appear in the first years of life: at just two years old, the child is extremely sensitive to ultraviolet rays of sunlight.
SKIN: SYMPTOMS AND SIGNS
The main symptoms of xeroderma pigmentosum occur in the skin. Patients show:
- Photosensitivity (i.e. an exaggerated reaction of the skin to sunlight)
- Tendency to tan easily, even after short exposures
- Numerous freckles already in the first years of life
- High predisposition to skin cancer
- Xeroderma
- Poikiloderma
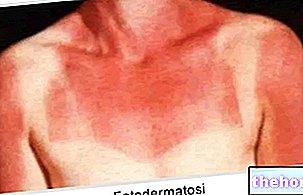
A healthy child, in the first years of life, tans with difficulty and almost never has freckles. A child with xeroderma pigmentosum, on the other hand, is extremely sensitive to UV rays (photosensitivity) and is subject to a rapid tan and the appearance of numerous freckles, especially in areas of skin exposed to the sun. The photosensitivity and the easy pigmentation of the skin are characteristics that certainly do not go unnoticed, as those affected show violent redness and skin lesions, even after a short exposure to the sun.
In a few years, then, the patient develops xeroderma, ie dryness and easy peeling of the skin, and poikiloderma, ie a "hyperpigmentation of certain regions of the skin.
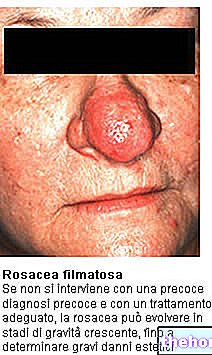
Finally, skin cancers are the most dramatic signs, also because they do not spare any individual with xeroderma pigmentosum. They are very precocious and can make their appearance, in patients who do not protect themselves adequately from the sun, as early as the 8th -10th year of life. The areas of the body most affected by cancer are the face, lips, eyelids. , the scalp and the tip of the tongue.
Why is it called xeroderma pigmentosum?
The term of xeroderma pigmentosum is due to two typical clinical signs of this disease: xeroderma and the tendency to tan easily (ie easy skin pigmentation).
THE EYES: SYMPTOMS AND SIGNS
The eyes of a patient of xeroderma pigmentosum are very sensitive to the ultraviolet rays of the sun; this is because, like skin, they lack protection. For the same reason they manifest photophobia and inflammation of the conjunctiva (conjunctivitis) and cornea (keratitis). They are also red, extremely irritated and predisposed to ocular tumors (malignant or not).
The eyelids, in addition to developing skin cancers, become unusually pigmented, completely lose their lashes, become atrophic and affected by ectropion or entropion.
In summary, the symptoms and signs at the ocular level are:
- Photophobia
- Inflammations of the conjunctiva
- Keratitis (inflammation of the cornea)
- Eye redness and irritation
- Eye tumors (malignant and non-malignant)
- Skin tumors of the eyelids
- Loss of eyelashes
- Atrophy of the eyelids, with phenomena of ectropion or entropion
NERVOUS SYSTEM: SYMPTOMS AND SIGNS
About 30% of people with xeroderma pigmentosum experience neurological disorders. These are very different symptoms, ranging from microcephaly to sensorineural hearing loss, from lack of coordination to movement difficulties, etc.
The following table summarizes the typical neurological signs of xeroderma pigmentosum.
Manifestations of xeroderma pigmentosum at the neurological level:
- Reduced or missed deep reflex of the tendons
- Sensorineural deafness (i.e. due to the lack of acoustic transmission of the nerve signal between the ear and the brain)
- Decline in cognitive functions
- Epilepsy
- Microcephaly
- Loss of coordination
- Difficulty moving, even just walking
- Difficulty speaking and swallowing
COMPLICATIONS
We have already talked about skin and eye cancers. However, these are not the only complications of xeroderma pigmentosum. A patient, in fact, is generally predisposed to many other cancers: for example, at the level of the buccal cavity, lungs and internal organs.
The reason is linked, as for damage to the skin and eyes, to the failure to repair damaged DNA, which afflicts all the cells of the organism, not just those exposed to UV rays.
To all this, it should be added, then, that there is a greater sensitivity to cigarette smoke (even passive one) and to chemical mutagens, even common ones.
For these reasons, sick individuals do not have a long life expectancy and must pay close attention to the time they spend exposed to the sun and in certain polluted environments.
Diagnosis
The diagnosis of xeroderma pigmentosum is based on the "clinical examination of the signs shown by the patient. D" on the other hand, it could not be otherwise, given that, as has been said, the skin manifestations (redness, lesions, appearance of freckles at an early age, xeroderma etc.) and ocular (keratitis, absence of eyelashes etc.) are quite evident and unambiguous.
EARLY DIAGNOSIS
Early diagnosis is very important, as recognizing xeroderma pigmentosum in time can delay, as far as possible, the onset of skin cancers and other complications.
It is quite easy to detect the disease in a child, as the appearance of freckles at the age of 2 is quite unusual.
In these cases, and at the slightest suspicion, it is advisable to contact your dermatologist immediately.
LABORATORY EXAMS
The laboratory test, which is most practiced if xeroderma pigmentosum is suspected, is skin biopsy. In fact, molecular biology investigations can be performed on a skin sample, which show the ability of skin cells to repair damage. DNA.
ARE THERE GENETIC TESTS?
Genetic tests, currently possible, concern only two types of pigmentary xeroderma: the "XPA and the" XPC. Molecular tests are used to recognize other types of xeroderma pigmentosum, which are not properly classified as genetic tests.
PRENATAL DIAGNOSIS
If a pregnant woman deems it appropriate, it is also possible to carry out a prenatal test (after sampling of amniotic fluid), to find out if the child is affected by xeroderma pigmentosum or not. However, given the rarity of the disease and the risks involved in taking an amniotic fluid sample, the doctor does not recommend this diagnostic test.
Treatment
Unfortunately, there is no cure for pigmentary xeroderma. In fact, the only possible therapeutic treatments are to be considered more than countermeasures to contain symptoms, rather than actual specific treatments.
The fundamental points of the therapy are:
- Avoid exposure to ultraviolet rays from the sun
- Continuous monitoring by the patient of their health conditions
- Medicines for symptom containment
- Surgical interventions against the largest and most serious tumors
- Psychological support
AVOID EXPOSURE TO UV RAYS
To avoid exposure to sunlight as much as possible, the patient is advised not to go out during the day, but only in the evening, when the sun has set;

to wear fully covering clothes, hats and sunglasses; to keep the haircut medium-long; regularly spread sunscreen cream on the skin; to apply special anti-UV glass to the windows of the house; to change those bulbs in the house that emit UV radiation with special lights, which do not emit them, etc.
A patient of xeroderma pigmentosum, who follows these indications, can develop a deficiency of vitamin D, the presence of which, in the human organism, is due precisely to sunlight.
CONTINUOUS MONITORING
Periodic checks are recommended at various specialists, to observe the progress of the disease. Every 3 months or so, it is advisable for the patient to see a dermatologist for a skin check.
It is also advisable, at least once a year, to undergo an ophthalmological examination to monitor the condition of the eyes.
Finally, neurological, hearing and vitamin D levels should not be forgotten.
PHARMACOLOGICAL TREATMENTS
Pharmacological treatments, provided for patients with xeroderma pigmentosum, include:
- Taking vitamin D supplements
They are used to cope with the inevitable deficiencies of this vitamin that our body synthesizes thanks to sunlight. - Emollient creams
They are used against xeroderma. - Artificial tears
They serve against dry eyes. - Oral isotretinoin
It is a drug against juvenile acne. It reduces photosensitivity and provides protection against redness and skin irritation. However, its use should be limited due to side effects.
SURGERY
Skin tumors and xeroderma very often require surgical / aesthetic interventions on the patient's skin. These interventions consist of skin transplants, using a dermatome, and dermabrasion interventions. The choice of the most opportune moment to intervene is up to the dermatologist, who will make a correct evaluation of the risks and benefits of the operation.
The same caution is also reserved for keratitis. In fact, corneal transplantation is performed when corneal inflammations are very severe.
PSYCHOLOGICAL SUPPORT
Individuals with xeroderma pigmentosum often suffer from depression. Among the causes of psychological distress, there are certainly behavioral restrictions, to which patients must scrupulously adhere, the aesthetic aspect and, in some cases, neurological disorders.
In these situations, psychological support and the proximity of closest family and friends are essential.
Prognosis
The prognosis of xeroderma pigmentosum is never positive. Those affected, in fact, are destined, sooner or later, to develop some form of cancer, in particular to the skin and eyes.
Furthermore, the scrupulous observance of certain behavioral limitations, such as never going out during the day, and the aesthetic appearance, altered by photosensitivity and ocular disorders, significantly influence the quality of life.
Unfortunately, the treatments of the moment do not provide results that will cure patients, but only relieve the symptoms. The advice, which is usually given to family members in these cases, is to stay close to the patient, providing him with psychological support and helping him to care for himself.







.jpg)


















