Generality
Testicular cancer, or testicular cancer, is a neoplastic process that originates in the cells (germinal or non-germinal) of the male gonads, called testes.

Figure: a seminoma. From wikipedia.org
The triggering causes have not yet been precisely delineated, however, thanks to the observation of a large number of cases, it was possible to ascertain that the neoplasm is linked to certain conditions, such as: cryptorchidism, familiarity with the tumor, infertility, smoking cigarette, tall stature etc.
The tumor process is characterized by the appearance of scrotal pain and a swelling in the testicles, the size of which is similar to that of a pea.
The diagnosis, if it is early, offers a good chance of recovery; healing that can be achieved with testicle removal surgery, chemotherapy and, in severe cases, even radiotherapy.
What is testicular cancer?
Testicular cancer, or testicular cancer, is an uncommon cancer that originates in the cells of one or both of the male gonads.
THE TESTICLES
The testes, or didymes, are the male gonads, therefore they represent the main reproductive organs of the male.
Contained in the scrotum, they are two in number and have the task of producing millions of spermatozoa, that is the man's sex cells, and the male sex hormones (testosterone). The latter are fundamental in the development of primary and secondary sexual characteristics. and in the control of the functions of the genital apparatus itself.
The size and weight of the testicles in adults:
- 3.5-4 cm in length
- 2.5 cm wide
- 3 cm in anteroposterior diameter
- 20 grams of weight approximately
TYPES OF TESTICLE CANCER
Depending on the type of testicular cells affected by the tumor, there are different forms of testicular cancer.
Approximately 95% of all testicular cancers originate in the cells from which spermatozoa, or germ cells, derive. Several subtypes belong to this category; of these, the main ones are seminomas and non-seminomas.
The remaining 5% is represented by tumors that originate in non-germinal testicular cells (or stromal cells). The so-called Sertoli cell tumor and the so-called Leydig cell tumor belong to this group of neoplasms.
EPIDEMIOLOGY
The t

It most frequently affects the young population, which is between 15 and 44 years of age, and with a white complexion (in particular, the inhabitants of Northern Europe, from Germany, Scandinavia, etc.).
According to an American study, since the "70s, testicular cancer patients around the world have increased in a decisive and inexplicable way. However, this increase has not translated into an increase in mortality, on the contrary, it has been noted a completely opposite trend, which can be explained by the advances made in medicine, which now guarantee a good chance of recovery from this neoplasm.
According to an Italian statistic, the cases registered in 2012 in our country were just over 2000.
Causes
Premise: what is a tumor? A tumor is the result of uncontrolled cell multiplication following one or more genetic DNA mutations.
The exact causes of testicular cancer are still unknown. However, several risk factors have been identified, some more significant than others, such as:
- Cryptorchidism
- Family history of testicular cancer
- Infertility
- Tall stature
- Cigarette smoke
- Belonging to Caucasian population (synonymous with white complexion) and young age
- Special chemical agents, such as pesticides, polychlorinated biphenyls and phthalates. These are also referred to as endocrine disruptors.
CRYPTORCHIDISM
When the male baby is still in the womb, his testicles are contained in the abdomen. After birth (precisely during the first year of life), they begin to descend and occupy the classic position inside the scrotum. However, on some occasions, this process of descent of the testicles does not occur or is incomplete: this situation it is termed cryptorchidism.
Of all the risk factors involved in the onset of testicular cancer, cryptorchidism is certainly the most influential.
For this reason, if a child is affected by cryptorchidism, it is essential to intervene as soon as possible with a specific surgery, in order to minimize the chances of developing a neoplasm.
American statistical research showed that the later cryptorchidism is corrected, the more likely testicular cancer is. For example, according to this study, if an individual undergoes corrective surgery after the 13th year of life, he may be up to 5 times more at risk than his healthy peers.
FAMILY HISTORY AND GENETICS
All people with close relatives (fathers or brothers) suffering from testicular cancer are at high risk of getting the same disease. Not surprisingly, familiarity is the second most important risk factor, after cryptorchidism.
As in the previous case, to get an "idea of the danger that the family members of a testicular cancer patient run, one must rely on statistical data: from these, it emerged that those who have (or have had) a sick father are 4 to 6 times more at risk than those who have (or have had) a healthy father.
According to some recent molecular biology studies, familiarity seems to be linked to a "genetic aberration, which affects the entire chromosome 12, and / or to various mutations, which affect the TGCT1, KITLG, SPRY4 genes.
INFERTILITY
For an unclear reason, it appears that male infertility predisposes to developing testicular cancer: in fact, infertile men are three times more at risk than fertile men.
HIGH STATURE
According to research from 2008, males over 190cm tall are prone to testicular cancer, while those less than 170cm are better protected. In light of this, the hypothesis has been advanced that there may be a connection between tall stature and testicular cancer. However, it remains to be explained what this link is due to.
SMOKE
As with many other cancers, testicular cancer is also favored by cigarette smoking. In fact, all heavy smokers are twice as at risk.
N.B: by heavy smokers, s "means all those who smoke, for years, even 20 cigarettes a day.
Symptoms and Complications
For further information: Symptoms Testicular cancer
Testicular cancer usually presents with a lump in one or both testicles. This swelling, which is painless on palpation, is a real bump, about the size of a pea or even larger.
In addition to this classic sign, other symptoms and disorders may appear, such as:
- Dull pain or sharp pain in the testicles or scrotum. That feeling comes and goes.
- Sensation of heaviness in the scrotum
- Dull pain in the abdomen
- Hydrocele, which is a collection of fluid, in the scrotum, all around the testicle
- Sense of fatigue
- Sense of general malaise
WHEN DO YOU CONTACT YOUR DOCTOR?
The appearance of a palpable and painless swelling, similar to that described above "on the contrary, does not necessarily mean that it is a testicular tumor. However, it is advisable to contact your doctor as soon as you notice its presence, as soon as possible the treatment of a possible tumor is begun, the more likely it is to recover from the neoplasm.

Figure: the size of a testicular tumor. It can be very small (T1), medium-sized (T2 and T3) or very large (T4). Greater magnitude is usually synonymous with greater severity. From the site: andrologiaurologiamontano.it
According to some statistics, less than 4% of swellings in the testicles are caused by testicular cancer; despite this, it is always better to undergo the most accurate checks.
COMPLICATIONS
Testicular cancer, when severe or not treated properly, can spread to other parts of the body; through the lymphatic or blood system, it can in fact invade, first, the neighboring lymph nodes and, subsequently, the more distant lymph nodes, the lungs, the liver, etc. This process, at its peak, is known as metastasis, and cancer cells that spread elsewhere are called metastases.
Diagnosis
To diagnose testicular cancer, the patient complaining of suspected disorders must be subjected to a series of different checks. It begins with a physical examination and a "scrotal ultrasound and ends with a" blood test and biopsy.
If there is concern that the tumor may have spread elsewhere (metastasizing), a series of more or less invasive radiological tests are also performed.
OBJECTIVE EXAMINATION
During the physical examination, the doctor analyzes the testicles, in particular the suspected swelling, also resorting to the use of a small torch. If light passes through the bump, it means that the scrotum contains fluid (most likely a cyst) and not a tumor. If the light, on the other hand, does not filter in, it is very likely that the swelling is caused by a solid mass, of tumor origin.
After examining the testicles, the doctor moves on to investigate the patient's medical history. If a past of cryptorchidism or a familiarity with the neoplasm emerges from it, the diagnosis already takes on well-defined contours.
SCROTAL ULTRASOUND
Scrotal ultrasound is a non-invasive diagnostic procedure that provides a wealth of useful information.
In fact, it shows the position and extent of the testicular anomaly and clarifies whether it is a collection of liquids or a solid mass.
As already mentioned, testicular cancer is suspected if the mass is solid, while the hypothesis of a cyst if there is an accumulation of fluid is considered.
BLOOD ANALYSIS
Blood tests are used to trace the so-called tumor markers in the bloodstream. These markers are nothing more than distinctive substances, which the tumor disperses in the circulating blood after forming. Their identification is very significant, however not all testicular cancers produce these markers. Therefore, the results of blood tests must always be taken with extreme caution.
Tumor markers, searched for in the blood:
- AFP (alphafetoprotein)
- HCG (chorionic gonadotropin)
- LDH (lactate dehydrogenase)
BIOPSY
The biopsy is performed to definitively confirm the actual presence of a testicular tumor. This examination involves taking a piece of tissue from the infected testicle and observing it under a microscope. On the instrument, tumor cells, if present, are easily recognizable.
Special case. When you are already certain of the diagnosis and / or when the risk of metastasis is concrete, the biopsy is performed on the entire testicle affected by the neoplasm. This means that the latter is completely removed (orchiectomy).
OTHER TESTS
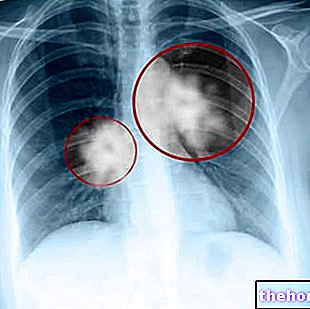
If you fear that the tumor will spread to the rest of the body, it is very useful to subject the patient to various radiological checks, which clarify whether the metastases have reached the lymph nodes, lungs, liver, etc.
The tests performed in these situations are: chest X-ray, nuclear magnetic resonance (MRI), computerized axial tomography (CT).
HOW IS THE SEVERITY OF A TESTICLE CANCER ESTABLISHED?
The severity of a testicular tumor depends on the characteristics it possesses, which are evaluated exclusively during the diagnostic process.
The factors that classify a tumor are the size of the tumor mass and the ability of tumor cells to spread.
Based on these characteristics, testicular cancer can be:
- Stage 1, if the cancer is confined to the affected testicle.
- Stage 2, if the cancer includes the affected testis and neighboring lymph nodes in the abdomen and pelvic area.
- Stage 3, if the cancer has spread from the testicle to the lymph nodes in the chest.
- Stage 4, if the cancer has spread not only to the lymph nodes in the chest, but also to the chest and abdomen organs, such as the lungs or liver.
Treatment

Figure: an interesting reproduction of the stages that characterize testicular cancer. It is possible to recognize the lymph nodes (blue-violet), lung metastases (yellow) and the kidney (the organ located just under the armpit, to the right of the reader) From the site: andrologiaurologiamontano.it
The only way to treat testicular cancer is to remove the entire affected testicle, using a surgery known as an orchiectomy.
This operation can be followed, depending on the stage and type of tumor, by the surgical removal of the abdominal lymph nodes and one or more cycles of chemotherapy and radiotherapy. These treatments have the aim of definitively eliminating the neoplastic cells from the organism.
If the testicular tumor is bilateral, after the removal of both testicles, the patient undergoes hormonal therapy, which restores erection capacity, but not fertility.
ORCHIECTOMY
For further information: Orchiectomy
The orchiectomy requires general anesthesia and is performed by making an incision at the inguinal level, through which the entire diseased testicle is removed from the scrotum.
The sooner the operation is performed, the lower the risk of the neoplasm invading the other testicle and other organs. This is why an early diagnosis of the disease is essential.
If the patient requests it, after the removal, the surgeon can place an artificial testicle made of silicone in place of the diseased testicle.
Key note on orchiectomy surgery. The removal of a testicle does not reduce and does not affect the patient's libido and fertility; these, in fact, remain unchanged.
Things, on the other hand, are very different if both testicles are removed (bilateral orchiectomy): in such situations, the production of testosterone and, above all, of spermatozoa (sterility) ceases.
SURGICAL REMOVAL OF AFFECTED LYMPH NODES
When the abdominal lymph nodes become contaminated with cancer (stage 2), they must be removed with surgery, to avoid the danger of the neoplasm returning. Generally, the removal of these small organs, which can be performed with various surgical techniques, has no particular side effects. However, in some cases, it can cause a disorder known as retrograde ejaculation.
CHEMOTHERAPY AND RADIOTHERAPY
Chemotherapy is the administration of drugs capable of killing all rapidly growing cells, including cancer cells. These preparations can be taken by mouth or intravenously.
Radiotherapy, on the other hand, consists of subjecting the patient to several cycles of ionizing radiation (high-energy X-rays), in order to destroy the tumor cells.
Chemotherapy and radiotherapy become essential when the tumor is severe and in an advanced stage: in fact, these treatments represent the only valid therapeutic solution, to remove tumor metastases from the body.
The main side effects of chemotherapy:
The main side effects of radiotherapy:
- Nausea
- He retched
- Hair loss
- Sense of fatigue
- Infection vulnerability
- Nausea
- Sense of fatigue
- Diarrhea
- Skin redness
- Predisposition to other cancers
TESTOSTERONE-BASED HORMONAL THERAPY
Patients, who have both testicles removed, must undergo hormone therapy based on synthetic testosterone if they want to maintain their libido and erectile abilities.
It should be remembered that hormonal treatment does not restore sperm production, as this last process is only made possible by the presence of the testicles.
For further information: Drugs to Treat Testicular Cancer "
Prognosis
Testicular cancer is a neoplasm that, if diagnosed early, can be treated with excellent results.
Starting from the 1970s, in fact, less and less people die from this pathology, so much so that, at the present time, 90% of patients (or 9 cases out of 10) recover completely.
In addition to the high percentage of cure, timely diagnosis (or early diagnosis) offers another big advantage: that of resorting to only one course of chemotherapy, also called surveillance, and nothing more. An advanced stage testicular cancer, on the other hand, it requires multiple courses of chemotherapy and, very often, radiotherapy as well.
FOLLOW UP
According to some statistical studies, 25-30% of patients cured of testicular cancer (the so-called follow-ups) undergo a relapse, or a reappearance of the neoplasm. This usually happens within the first two years after the end of therapy. Therefore, it is highly recommended that you undergo periodic diagnostic tests and checks during this time
- Four controls, during the first post-operative year
- Two checks, during the second post-surgery year
- An annual check-up, starting from the third post-surgery year
PREVENTION
Testicular cancer cannot be prevented, however, with periodic self-examination of the testicles (the ideal time is after a hot shower), it is possible to detect some anomaly by oneself.
This indication, together with that of not smoking, is particularly recommended for all those who have a history of cryptorchidism or a family history of testicular cancer.