Generality
Gram-positives are bacteria which - as can be deduced from their name - test positive for Gram stain retaining a purple color after having undergone such laboratory analysis.

Bacterial cell wall
The bacterial cell wall can be defined as a sort of rigid "container" that encloses the bacterial cell, giving it a certain strength and conditioning its shape.
The fundamental component of the cell wall is the peptidoglycan (otherwise known as bacterial mucopeptide or murein).
Peptidoglycan is a polymer consisting of long linear polysaccharide chains, joined together by cross-links between amino acid residues.
Polysaccharide chains are composed of the repetition of a disaccharide, which in turn consists of two monosaccharides, the N-acetylglucosamine (or NAG) and acid N-acetylmuramic (or NAM), linked together by β-1,6 glycosidic bonds.
The disaccharides are then linked to each other with β-1,4 type glycosidic bonds.
Linked to each molecule of NAM we find a pentapeptide (ie a "tail" of five amino acids) ending with two equal amino acids, in particular, with two molecules of D-Alanine.
It is precisely these terminal D-Alanine which - following the action of the transpeptidase enzyme - allow the formation of cross-links within the peptidoglycan.
More precisely, the transpeptidase originates a peptide bond between the third amino acid of a polysaccharide chain and the fourth amino acid of the parallel polysaccharide chain.

Functions
The cell wall not only exerts a protective role towards the bacterial cell but also regulates the transport of substances inside it.
Therefore, it can be said that the main functions of the cell wall are:
- Prevent breakdown of bacterial cells due to osmotic pressure. In fact, very often, bacteria live in hypotonic environments, that is, in environments where large quantities of water are present and which are "more diluted" than the internal environment of the bacterial cell. This difference in concentration causes the water pass from the external environment (less concentrated) to the inside of the bacterial cell (more concentrated) in an attempt to equalize the concentration between the two environments. The uncontrolled entry of water would cause the bacterial cell to swell until it burst (osmotic lysis).
The function of the cell wall is precisely that of resisting the external pressure of water, thus preventing swelling and bacterial lysis. - Protect the plasma membrane and the cellular environment from molecules or substances harmful to the bacteria itself.
- Regulate the entry of nutrients into the bacterial cell.
Everything described so far can be found both in the Gram-positive and in the Gram-negative walls.
However, since the purpose of this article is to clarify the peculiarities of Gram-positive bacteria, only the characteristics of the cell wall of the latter will be described below and the Gram-negative wall will not be considered.
Gram-positive cell wall
In the Gram-positive wall, the peptide bond between the polysaccharide chains of the peptidoglycan is formed through a pentaglycine bridge, that is, a bridge consisting of five molecules of glycine (an amino acid).
The cell wall of Gram-positive is uniform and relatively thick (20-80 nm). It consists of numerous peptidoglycan layers that are intersected by theic acids (polymers of alcohols and phosphates).
The Gram-positive wall is very polar and allows the permeation of hydrophilic molecules (such as those used in the Gram stain which will be described below) but not of hydrophobic compounds.

Gram stain
Gram staining is a process devised and developed in 1884 by a Danish bacteriologist, Hans Christian Gram.
The first step of this procedure involves the preparation of a smear (ie a thin film of the material to be analyzed) fixed by heat. In other words, a sample of the bacteria to be analyzed is placed on a slide and - through the use of heat - the microorganisms are killed and blocked on the slide itself (hot fixation). After preparing the smear, you can proceed with the actual staining.
The Gram stain technique has four main steps.
Phase 1
The heat-fixed smear should be coated with the dye crystal violet (also known as gentian violet) for three minutes. By doing this, all the bacterial cells will turn purple.
Phase 2
At this point, la Lugol's solution (an aqueous solution of iodine and potassium iodide, defined as a mordant, since it is able to fix the color) and is left to act for about a minute.
Lugol's solution is polar and penetrates the bacterial cell where it meets the crystal violet with which it forms a hydrophobic complex.
Since the Gram-positive cell wall is polar, the crystal violet-iodine hydrophobic complex cannot cross it, thus remaining locked inside the bacterial cell itself.
Phase 3
The slide is washed with a bleach (usually alcohol or acetone) for about twenty seconds. After that, it is washed with water to stop the action of the bleaching agent.
At the end of this phase, the Gram-positive bacteria cells will have retained the purple color.
The Gram-negative cells, on the other hand, will have discolored. This happens because the alcohol attacks the lipopolysaccharide structure of the external membrane typical of Gram-negative and absent in Gram-positive, thus facilitating the loss of the previously absorbed dye.
Phase 4
A second dye is added to the slide (usually, acid fuchsin or safranin) and let it act for a couple of minutes.
At the end of this phase, the cells of Gram-negative bacteria that have undergone discoloration in the previous phase, will take on a color ranging from pink to red.
Types of Gram-positive bacteria
The large Gram positive group includes many bacterial species.
Below, some of the bacteria belonging to this large category will be briefly listed.
Staphylococci (or Staphylococcus)
Staphylococci are cocci (i.e. spherical bacteria) belonging to the family of Staphylococcaceae. Staphylococci grow in clusters.
Among the various types of pathogenic staphylococci, we remember:
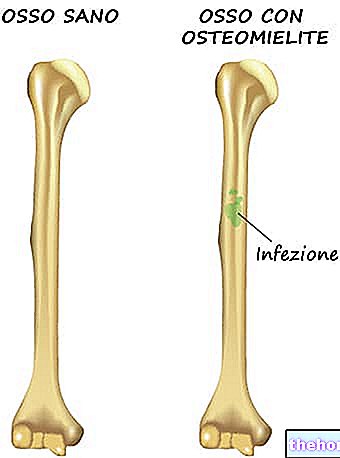
- Staphylococcus aureus, responsible for various infections of the genitourinary tract, the neural system, the skin, the bones, the joints, the cardiovascular system, the respiratory tract and the eye. Furthermore, this beating is also responsible for associated opportunistic infections compromising the host's immune system, nosocomial opportunistic infections (ie infections contracted within health facilities) and food poisoning.
- Staphylococcus epidermidis, responsible for "infections of the cardiovascular system," opportunistic infections associated with compromised immune system of the host and "nosocomial opportunistic infections.
- Staphylococcus saprophyticusresponsible for urinary tract infections.
Generally, antibiotics such as penicillins, vancomycin, daptomycin, cephalosporins or fluoroquinolones are used against this type of bacteria.
Streptococcus (or Streptococcus)
Streptococci are cocci that grow in pairs or in chains. Streptococci are capable of producing toxins capable of destroying red blood cells, that is, they are endowed with haemolytic activity.
Streptococci can in turn be subdivided according to the degree of hemolysis they induce. Therefore, we can distinguish:
- Streptococci alpha-haemolytics (or α-haemolytics) that cause "partial haemolysis;
- Streptococci beta-haemolytics (or β-haemolytics) that cause "total haemolysis;
- Streptococci gamma-haemolytics (or γ-haemolytics) that do not cause haemolysis.
Among the pathogenic streptococci, we remember:
- Streptococcus pyogenes, responsible for infections of the respiratory tract, skin, bones, joints, cardiovascular system, digestive glands and peritoneal cavity. Furthermore, it is also responsible for opportunistic infections in hosts with compromised immune systems.
- Streptococcus agalactiaeresponsible for infections in the fetus and newborn, infections of the nervous system and respiratory tract.
- Streptococcus pneumoniae, responsible for infections of the respiratory tract, the nervous system, the cardiovascular system, the digestive glands, the peritoneal cavity and opportunistic infections associated with compromising the host's immune system.
Usually, beta-lactam and macrolide antibiotics are used against streptococci.
Clostridia (or Clostridium)
Clostridia are bacilli (ie cylindrical-shaped bacteria) which - in adverse environmental conditions - are able to generate spores in order to survive.
Among the various existing pathogenic clostridia, we remember:
- Clostridium difficile, this bacteria can be part of the normal human bacterial flora and is responsible for opportunistic infections of the gastrointestinal tract. It is the main cause of pseudomembranous colitis which can arise in patients treated for a long time and at high doses with antibiotic drugs of various types. Against infections from Clostridium difficileantibiotics such as metronidazole, chloramphenicol, vancomycin or erythromycin are usually used.
- Clostridium tetani, responsible of tetanus (or spastic paralysis). Generally, metronidazole or benzylpenicillin are used against this beating. A vaccine is also available to prevent infection.
- Clostridium botulinum, responsible of botulism (or flaccid paralysis).
Corinebacteria (or Corynebacterium)
Corinebacteria are bacilli belonging to the family of Corynenacteriaceae.
Among the numerous exponents of this genre, we remember the Corynebacterium diphteriae responsible for cutaneous diphtheria and respiratory diphtheria.
The antibiotics usually used to treat diphtheria are penicillins, cephalosporins, clindamycin and erythromycin.
A vaccine is also available to prevent infection.
Other Gram-positives
Other Gram-positive bacteria are:
- Bacillus anthracis (known as anthrax), responsible for the onset of cutaneous, pulmonary and gastrointestinal anthrax;
- Listeria monocytogenes, a bacillus responsible for the onset of meningitis, encephalitis, meningoencephalitis and brain abscesses;
- Enterococcus faecium and Enterococcus faecalis, two cocci which normally populate the human intestinal bacterial flora, but which may be responsible for nosocomial opportunistic infections of the urinary tract, septicemias or endocarditis.