To induce the phenomenon of antral gastritis are the sudden weakening of the mucus layer, which covers the internal surface of the stomach, and the simultaneous erosive action, on the aforesaid surface, exerted by the acid juices necessary for the digestive process.
Among the main causes of acute gastritis (and of the upheavals just described), there are: infections caused by Helicobacter pylori, the abuse of common drugs such as NSAIDs, alcoholic substance abuse and excessive psychophysical stress.
As a rule, to properly treat a condition such as acute gastritis, a "thorough diagnostic investigation is essential, which brings to light the triggering causes.
Brief review of the term Gastritis
In medicine, "gastritis" is the word for inflammation of the inner wall of the stomach.
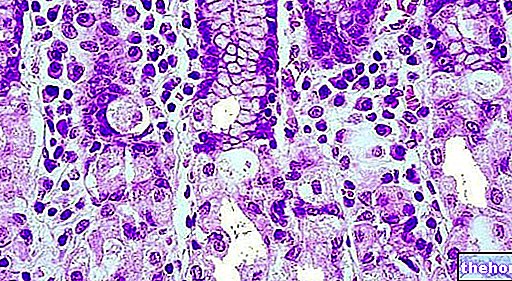
Also known as the internal gastric mucosa, the internal wall of the stomach is the complex of cell layers responsible for:
- The production of acidic digestive juices, necessary for the digestive process;
- The secretion of mucus intended to protect the stomach from the aforementioned acid digestive juices;
- The production of the gastrin hormone.
Secretes protective mucus.
It has a dense network of glands, responsible for the production of acidic digestive juices.
It contains muscle cells, which guarantee the stomach the ability to move food towards the intestine and proceed with the digestive process.
Acute gastritis is opposed to chronic gastritis. With the expression "chronic gastritis", doctors mean the "inflammation of the internal part of the stomach with gradual onset, mild in terms of symptoms, lasting several weeks and possibly leading to relapses.
Are Acute Gastritis and Gastroenteritis the Same Thing?
Acute gastritis should not be confused with gastroenteritis. The latter, in fact, is the condition resulting from the simultaneous inflammation of the internal wall of the stomach and intestine.
The fact that gastroenteritis also affects the intestine is the explanation for the presence of diarrhea, a symptom which, as will be seen, is absent in acute gastritis.
In other words, acute gastritis is the consequence of the damage that the acidic digestive juices of the stomach cause to the internal gastric mucosa, when the latter loses part of its protective mucus layer.
Did you know that ...
When gastritis, whether acute or chronic, affects the inner wall of the stomach in its entirety or almost, it is called pangastritis.
Causal Factors of Acute Gastritis
To suddenly weaken the protective mucus layer of the stomach and consequently to cause / promote acute gastritis can be various factors and conditions; more specifically, the causes / risk factors of acute gastritis include:
- Infections sustained by Helicobacter pylori. Helicobacter pylori it is a bacterium normally present inside the stomach (it tolerates the acidic environment very well) and has no consequences for health. If, however, the immune defenses of the human organism lose their effectiveness, this microorganism is free to proliferate in an uncontrolled way and colonize its host, causing an infection.
Favored by cigarette smoking and high psychophysical stress, infection with Helicobacter pylori it is most likely the main causative factor of antral gastritis; - Prolonged and improper use of certain drugs, such as NSAIDs (eg aspirin, ibuprofen, naproxen, etc.), chemotherapy drugs (eg mitomycin and floxuridine) and colchicine;
- Prolonged abuse of alcoholic beverages (especially whiskey, vodka and gin);

Shutterstock Helicobacter pylori
- The use of drugs such as cocaine;
- A diet having the undesirable effect of elevating the acidity of the stomach. Such a diet generally consists in the excessive consumption of: fats, cooked oils, citrus fruits and coffee;
- Some viral infections, such as cytomegalovirus infections and AIDS;
- Some fungal infections, such as candidiasis (or candidiasis), histoplasmosis or zygomycosis;
- Some parasitic infections (or parasites), such as anisakiasis;
- Radiation therapy performed for the treatment of a tumor;
- Very intense stress. Stressful circumstances to the point of favoring acute gastritis are, just to mention a few examples, major surgery, chronic diseases and serious injuries.
Acute or chronic forms of gastritis that are the result of stress are examples of nervous gastritis. - Bile reflux. Biliary reflux is the ascent of bile from the duodenum to the stomach and, in the most severe cases, also to the esophagus;
- Gastric ischemia. Ischemia is the medical term that indicates a more or less severe reduction in the flow of blood in a certain tissue or organ, such a reduction as to cause a drop in the supply of oxygen and nutrients.
Gastric ischemia is ischemia located in the stomach; - Food allergies and food poisoning.
Who is most at risk for Acute Gastritis?
Also deductible in part from what has just been stated regarding the causal and triggering factors, the individuals most predisposed to developing acute gastritis are:
- Heavy consumers of alcoholic beverages;
- Who makes a lot of use of NSAIDs;
- Users of drugs such as cocaine;
- People undergoing major surgery;
- People with kidney failure;
- Subjects with hepatic insufficiency;
- Who suffers from respiratory failure.
Types of Acute Gastritis
There are two forms of acute gastritis: a less severe form, called acute non-erosive gastritis (or acute superficial gastritis), and a more severe form, called acute erosive gastritis.
ACUTE NON-EROSIVE (OR SURFACE) GASTRITIS
Acute non-erosive gastritis is the least severe form of acute gastritis; this condition represents, in fact, a suffering limited to the most superficial cells of the epithelium which constitutes the internal wall of the stomach (remember that the aforementioned epithelium is the cellular layer in direct contact with the lumen of the stomach).
ACUTE EROSIVE GASTRITIS
Acute erosive gastritis is the most severe form of acute gastritis; as a result of its presence, in fact, it is possible to observe scar-like lesions (ulcers) on the internal wall of the stomach as well as a significant decrease in the number of glands responsible for the production of acid digestive juices.
Acute erosive gastritis is a clinically delicate condition and therefore requires appropriate treatment.
- Indigestion (or indigestion). It is the most characteristic manifestation of acute gastritis.
Its presence is the result of the inevitable interference that inflammation produces towards the digestive process at the gastric level and the emptying of the stomach; - Stomach ache. To highlight this symptom is a pain localized in the upper part of the abdomen (epigastric pain), the intensity of which varies from patient to patient.
At the base of heartburn there is a noticeable increase in the levels of gastric acidity (or stomach acidity);

- Nausea, vomiting and loss of appetite. These are the three classic symptoms that accompany indigestion; therefore, they represent three quite common manifestations of acute gastritis.
Among these disorders there is the following relationship: nausea triggers vomiting and vomiting induces a decrease in appetite; - Flatulence and a sense of abdominal bloating and / or abdominal heaviness. Flatulence and abdominal bloating / heaviness depend, once again, on the bad digestive process; bad digestion, in fact, causes the food to reach the intestine only partially digested and this causes its fermentation (which is the real cause of flatulence and the sense of bloating / abdominal heaviness);
- General malaise and a sense of weakness. They are the direct consequences of the previous symptoms.
Complications of Acute Gastritis
In more severe cases or in the absence of adequate treatment, acute gastritis can degenerate to the point of inducing the formation of peptic perforating ulcers. In the medical field, perforating peptic ulcer is the expression that indicates any lesion of the digestive mucosa that has reached so deep that it has compromised the integrity of the underlying blood vessels and caused blood loss (gastrointestinal haemorrhage).
The classic manifestations of a perforating peptic ulcer are: persistent pain in the abdomen, black stools due to the presence of blood, blood loss from the rectum and vomiting with blood (haematemesis).
It should also be noted that cases of acute gastritis characterized by intense vomiting can, in the absence of treatment, establish a condition of dehydration with no negligible consequences.
When to see a doctor?
An individual should contact their treating physician, when suffering from the above symptoms for several consecutive days, with no hint of improvement.
In case of complications, it is a good idea to go immediately to the nearest medical-hospital center and undergo all the necessary treatments.
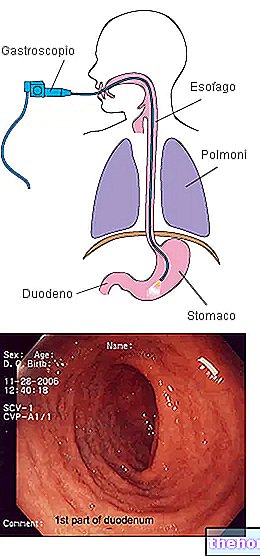
However, it happens quite frequently that the diagnostician wants to confirm and / or investigate the situation (for example discover the causes), consequently he also resorts to:
- The test for the tracing of Helicobacter pylori in the organism. It is a fairly common investigation, as this bacterium is the main cause of acute gastritis;
- Blood tests. Provides information on the patient's general health status;
- The stool test. It is used to establish if there is blood in the stool;
- Digestive endoscopy. It allows the doctor to view the inside of the stomach and understand the actual state of health of the mucosa;
- The x-ray of the digestive system with barium sulphate contrast medium. It is used to establish the general health of the patient's digestive system.
Why is a more thorough diagnosis useful?
Deepening the diagnosis of acute gastritis with further investigations allows us to discover its causes and risk factors.
Knowledge of the causes and risk factors is fundamental for planning the most appropriate therapy and for preventive purposes (as regards, of course, the prevention of relapses).
Symptomatic drug therapy
Medicines for the symptomatic therapy of acute gastritis are medicines for the control and limitation of gastric acidity.
Specifically, these drugs consist of:
- Antacids. They are useful for buffering gastric acidity and relieving heartburn, resulting from poor digestion.
Often, doctors associate them with the next two drug categories.
Examples of antacids classically used in the presence of acute gastritis are: magnesium hydrate and aluminum hydroxide. - Anti-H2 (or H2 receptor antagonists). They have the effect of reducing the stomach's production of acidic digestive juices.
Typical H2 blockers used in acute gastritis are cimetidine and famotidine. - Proton pump inhibitors (PPIs). They act similarly to H2 blockers, so they reduce the production of acid secretions in the stomach.
The classic PPIs administered during the management of acute gastritis are esomeprazole and omeprazole.
Recommended Diet Plan

In the presence of acute gastritis, the foods to avoid are: fried foods (because they contain a high percentage of fat), fatty foods, citrus juices, coffee and alcohol; the recommended foods are: all vegetables, fruit (except citrus fruits, of course), low-fat food products, lean meats (e.g. chicken or turkey meat), pasta and rice (NB: pasta and rice prepared, obviously, in a "light" way).
In the context of acute gastritis, careful dietary control can have unexpected beneficial effects.
Therapy in milder cases
In milder cases of acute gastritis, the indicated treatment is limited to the control of the diet, which must have the characteristics mentioned above (abolition of fatty foods, fried foods, coffee, etc.).