Generality
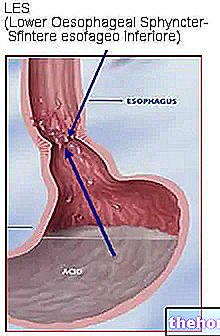
Esophageal achalasia is a motility disorder affecting the esophagus. The disease is caused by the lack of peristalsis and an incomplete opening of the lower esophageal sphincter (muscular valve located between the esophagus and the stomach) during swallowing.

The most common form, primary achalasia, is caused by abnormal smooth muscle innervation of the esophagus in the absence of other pathological conditions. However, a small percentage of cases occur as a secondary form of other pathologies, such as esophageal cancer or Chagas disease. There is no sex predominance and the onset of the disease occurs mainly in adults aged between 20 and 40 years of both sexes. Diagnosis is defined by radiographic studies with barium and esophageal manometry. Some medications or botulinum toxin injections can provide temporary relief for mild or moderate cases of esophageal achalasia, while the most effective and lasting intervention involves endoscopic therapy (esophageal balloon dilation) or surgical procedures (such as Heller's myotomy).
Esophagus, achalasia and swallowing
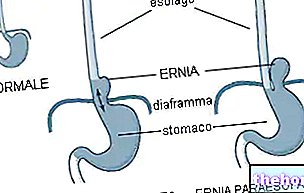
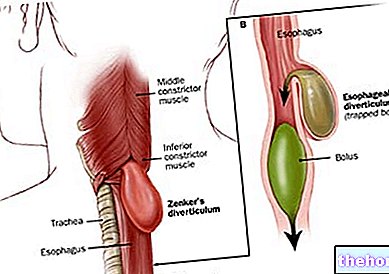
- The esophagus is a muscular tube that connects the pharynx to the stomach; inside this hollow organ, the bolus transits pushed by peristaltic movements, ie by rhythmic waves of involuntary muscle contractions. Peristalsis involves the contraction of the esophageal tract that precedes the bolus (upstream) and the relaxation of the following tract (downstream), in order to determine the rapid advancement of food from the esophagus to the stomach.
- The lower esophageal sphincter is a valve interposed between the terminal part of the esophagus and the initial part of the stomach; it has the function of preventing the reflux of acid gastric contents into the esophagus, opening only to allow food to pass during swallowing or vomit.
- Esophageal achalasia is a motor disorder characterized by the loss or alteration of peristalsis and failure to relax the lower esophageal sphincter when swallowing.
- Achalasia does not involve the upper esophageal sphincter and pharynx, so the patient can eat and swallow, but the bolus can easily stop along the esophagus. It follows: vomiting of undigested food, chest pain, heartburn and weight loss.
Slowly, over a number of years, people with esophageal achalasia experience an increasing difficulty in swallowing solid and liquid foods. If it progresses, the disease can cause considerable weight loss, anemia and malnutrition. In addition, as the condition progresses, the esophagus may deform, elongating or dilating. Patients with achalasia also have a slightly increased risk of developing esophageal cancer, particularly if the obstruction is present for a long time Your doctor may periodically recommend endoscopic checkups for the prevention and early diagnosis of esophageal carcinoma.
Causes
The causes of esophageal achalasia are not yet defined, but it is believed that a neurogenic deficit exists at the base, ie damage to the neurons responsible for peristalsis in the esophagus wall. Under normal conditions, the nerves coordinate relaxation, the opening of the sphincters (upper and lower) and peristaltic waves in the esophageal body.
Recent studies show that achalasia is caused by an alteration of some cells of the involuntary nervous system located inside the muscular layers of the esophagus. These are attacked by the patient's immune system and slowly degenerate, for reasons not currently understood. As the disease progresses, the nerves begin to degenerate, progressively involving muscle function as well. The result is the inability to get food down through the alimentary canal.
Furthermore, the etiology of esophageal achalasia could be linked to a previous infection. In particular, the disorder appears to be common in individuals with Chagas disease, caused by Trypanosoma cruzii.
There is no evidence to suggest a possible hereditary origin or transmission.
Signs and symptoms
Achalasia is a persistent problem that can cause symptoms that last for months or years. People who suffer from only a brief symptomatic episode, such as difficulty swallowing, generally do not have an actual disorder. of esophageal motility.
Symptoms of achalasia can begin at any time in life and usually come on gradually.
Most people with achalasia initially suffer from dysphagia, a condition in which it is difficult and sometimes painful to swallow food. This condition tends to get worse over the course of a couple of years. Dysphagia can cause: regurgitation of undigested food shortly after meals, choking, chest pain and heartburn. Some people may also experience coughing fits when lying flat. Pain in the chest (behind the breastbone) is also known as cardiospasm and can often be mistaken for a heart attack. From this point of view, achalasia can be extremely painful in some patients.
Dysphagia tends to progressively worsen over time.
In the later stage of the disease, when the esophagus is deformed by dilating, dysphagia occurs to a lesser extent (food no longer stops after swallowing it), but new symptoms arise such as frequent belching.
Finally, in the most advanced phase, dysphagia occurs again, so as to induce a gradual but significant weight reduction, the onset of anemia and the regurgitation of food not ingested. Both solid foods and liquids, including saliva or mucus, are blocked in the esophagus and can be inhaled into the lungs. lung infections, such as aspiration pneumonia.
In some people, esophageal achalasia causes no symptoms and is only discovered when a chest X-ray is taken or other investigations are conducted for another reason.
The main symptoms of esophageal achalasia include:
- Difficulty swallowing liquids and solids (dysphagia);
- Regurgitation of ingested food (especially at night);
- Chest pain, which may increase after eating
- Heartburn (retrosternal burning);
- Sialorrhea (excessive salivation) and halitosis;
- Cough and impaired respiratory function;
- Weight loss.
Possible complications of esophageal achalasia are:
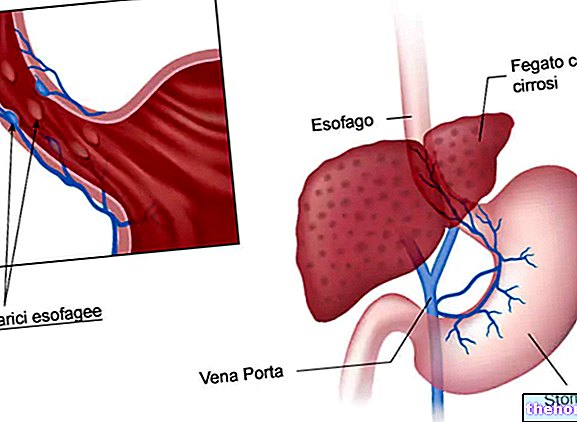
- Acid reflux from the stomach into the esophagus;
- Esophagitis;
- Infection in the lungs and aspiration pneumonia;
- Perforation of the esophagus;
- Cancer of the esophagus (achalasia correlates with a slightly increased risk).
Diagnosis
Three tests are most commonly used to diagnose and evaluate esophageal achalasia:
- X-ray with barium. A sequence of radiographic images is taken after the patient has ingested a barium-based preparation. In the presence of achalasia, peristaltic movement through the esophagus is not normal and is associated with a delay in the passage of barium. in the stomach. A traditional chest X-ray can show the deformity of the esophagus.
- Endoscopy. A flexible instrument, called an endoscope, is introduced from the mouth to allow the doctor to directly observe the morphology of the esophagus and stomach.
- Esophageal manometry. This investigation evaluates esophageal function and, due to its sensitivity, provides diagnostic confirmation: it measures the time and strength of the peristaltic esophageal waves and the contractions at the level of the lower esophageal sphincter. A thin plastic tube is inserted through the nose or mouth. The probe measures muscle contractions in different parts of the esophagus during swallowing. In case of achalasia, manometry reveals the inability of the lower esophageal sphincter to relax with swallowing and the lack of functional peristalsis of the smooth muscle of the esophagus .
Treatment
Treatment of esophageal achalasia aims to reduce the pressure within the lower esophageal sphincter to allow for easier passage of food from the esophagus to the stomach. The underlying disease cannot be cured, but there are various ways to improve symptoms.
Treatments for esophageal achalasia include:
- Medicines taken orally, which help relax the lower esophageal sphincter
- Balloon dilation (stretching of the lower esophageal sphincter)
- Laparoscopic Heller's esophagotomy or myotomy (surgical procedures that cut the muscle at the lower end of the esophageal sphincter);
- Botulinum toxin injection (Botox®).