Generality
Esophageal varices are abnormal, circumscribed and usually multiple dilations of the submucosal veins of the esophagus, in particular of its lower third. Typical consequence of portal hypertension, esophageal varices have a congenital origin only in a small percentage of cases; more often, they are known to embody one of the most fearful complications of liver cirrhosis; in fact, if not properly treated, esophageal varices can rupture, causing very serious bleeding, lethal in one in five patients.

Causes
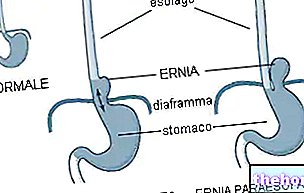
Understanding the pathogenesis of esophageal varices cannot be separated from the "in-depth knowledge of the anatomy of the venous system" of the organism. Simplifying the concepts as much as possible, we recall how the portal vein has the task of conveying the blood from the spleen, pancreas and liver to the liver. from the intestine. When the blood circulation of the liver is compromised and the blood struggles to flow inside and out - pouring into the hepatic veins (whose job is to bring it back to the heart through the inferior vena cava) - the pressure inside the portal vein In this case, we speak of portal hypertension. If we imagine a rubber hose to water and compare it to the portal vein, then in the presence of portal hypertension we must think of a plug that prevents the water from escaping from the hose: if we do not close the faucet in time, the pressure of the water in the hose will exhaust the walls until it explodes.
The most common causes of esophageal varices:
- Cirrhosis (scarring of the liver)
- Congenital intrahepatic scarring or obstructive processes
- Thrombosis (presence of clots obstructing the portal vein, splenic vein or hepatic veins)
- Schistosomiasis (parasitic infection typical of tropical countries)
- In Italy, over 90% of portal hypertension is due to liver cirrhosis
Fortunately, nature has equipped the human body with defensive mechanisms to avoid the tragic rupture of its vessels; once again we must use the imagination to compare the circulatory system to an intricate network of vessels, similar to the disordered meshes of a network: if the outflow of blood along a vessel is blocked or excessively increases the amount of blood flowing into it. circulates, there are collateral routes that can bypass the obstacle. Thus, in the presence of portal hypertension the bursting of the vein is prevented by the diversion of blood into other venous branches, which guarantee its return to the heart. collaterals try in some way to adapt to accommodate the greatest amount of blood that pervades them. In particular, at the level of the gastroesophageal junction, the submucosal veins swell up to become real varicose dilations: esophageal varices. A similar situation occurs. in the haemorrhoidal area, with the formation of anorectal varices, better known as haemorrhoids.
Symptoms
For further information: Esophageal Varic Symptoms
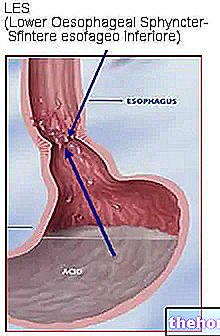
Esophageal varices manifest themselves with difficulty in swallowing (dysphagia), but the most characteristic and dangerous sign is represented by bleeding, signaled by the emission of blood through vomiting (haematemesis) or through the faeces (melaena: the blood, being digested, has a tarry consistency). It is assumed that the rupture of the esophageal varices is the consequence of the ascent of gastric juices along the esophagus (regurgitation or reflux), whose acidity erodes the esophageal mucosa.
To the typical symptoms of the varices of the esophagus are added those of the underlying disease, for example those deriving from cirrhosis (jaundice, vomiting, hepatic pain, edema, splenomegaly, ascites).
Diagnosis and Treatment
For further information: Medicines for the treatment of esophageal varices
The endoscopic examination through esophagus-gastro-duodenoscopy allows to observe the appearance of the varices, which is important for their classification and the assessment of the risk of rupture. This test is usually given to patients who have unexplained upper digestive tract bleeding.
Based on the appearance of the esophageal varices and the patient's general health, the physician may prescribe non-cardioselective beta blocking drugs such as propranolol and nadolol to contain portal hypertension.
Nitro-derivatives are also used for this purpose.
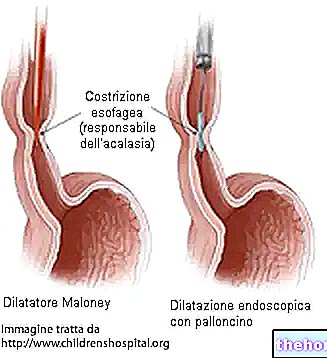
If the risk of bleeding from esophageal varices is important, the doctor proceeds to ligate them by means of (operative) esophagus-gastro-duodenoscopy, "strangling" them by means of rubber rings that constrict the veins, closing them and making them gradually disappear.
An alternative to ligation is the sclerosis of the same, which occurs through the injection of substances capable of inducing the formation of clots inside the varicose veins. To completely close all dilated veins, several treatments may be necessary; then repeated every 2-3 weeks until the esophageal varices disappear.
An alternative to these treatments consists in the decompression of the portal system by means of porto-systemic shunts: in practice, artificial venous bridges are surgically inserted that drain the blood from the portal vein to the vena cava bypassing the liver.