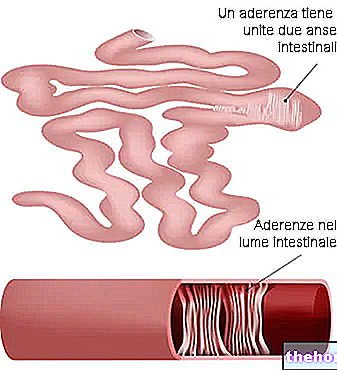
Diverticulitis is a disease of the colon. It represents the complication of an anatomical defect called diverticulosis, characterized by the formation of multiple intestinal diverticula.
Diverticula are pockets that form inside the colon. These invaginations (which can also affect other districts of the digestive tract) consist of the recess of the mucosa, the serosa and sometimes the muscular layer. The introflexion sites are mainly the passage orifices. of blood vessels.

When diverticula become infected / inflamed it is called diverticulitis.
The causes of diverticulosis and diverticulitis are not entirely clear. It is hypothesized that they have a genetic basis emphasized by some behavioral factors (diet and comorbidities).
(relapsing diverticulitis affecting many diverticula).
- Abdominal discomfort, pain or cramps after eating.
- They occur mainly after eating certain foods.
- Meteorism and flatulence.
- Diarrhea or constipation.
- Pain localized on the left side.
- In severe cases:
- Fever.
- More intense pains.
- Bleeding complications.
NB: Diverticula and diverticulosis are asymptomatic.
- Contact your doctor or gastroenterologist for an accurate diagnosis and treatment. After a "physical examination, they will order tests to confirm the suspicion of diverticulitis:
- Abdominal ultrasound.
- Computed tomography.
- Colonoscopy.
NB: The therapy of diverticulitis is aimed at reducing the possibility of acuteness or possibly at treating them. However, the diverticula cannot be eliminated and remain in the intestine for the entire life of the subject.
- First of all it is essential to stop smoking, drinking alcohol and possibly exposing yourself to toxic substances (of any kind).
- Particular attention should be paid to chewing, to avoid leaving indigestible solid pieces in the colon.
- The remedies for diverticulitis can be differentiated into:
- Diet and drug therapy for diverticulosis, diverticulitis prevention and mild infection.
- Diet and drug therapy for severe diverticulitis.
- Surgery for severe diverticulitis and complications (e.g. diverticular abscess, perforation and peritonitis).
NB: A recent study denies the correlation between higher fiber consumption and lower incidence of diverticulitis. Nonetheless, constipation remains the main risk factor in the formation of acquired diverticula.
- Liquid foods, free of any fixed residue.
NB: Artificial nutrition will follow after surgery.
.
NB: It is not advisable to eliminate fats from the diet as they have a lubricating effect in the intestine, facilitating evacuation and preventing constipation.
and supplements:- Plants or laxative extracts based on soluble fiber (NOT irritating):
- Psyllium seeds and extracted fiber.
- Amorphophallus konjac and glucomannans extracts.
- Gums: Guar, karaya etc.
- Mucilage: for example agar agar.
- Probiotic supplements.
- Supplements of anti-inflammatory and antioxidant molecules: the correlation with diverticulitis is unknown, but they could help reduce inflammation: omega 3, polyphenolic antioxidants, vitamin antioxidants (A, C, E) and mineral antioxidants (zinc and selenium).
- Systemic antibiotics:
- Ciprofloxacin (e.g. Ciprofloxac, Samper, Ciproxin, Kinox).
- Metronidazole (e.g. Metronid, Deflamon, Flagyl).
- Clindamycin (e.g. Dalacin-T, Clindamycin BIN, Zindaclin, Dalacin-C).
- Drug combinations such as Sulfamethoxazole / Trimethoprim (e.g. Bactrim).
- Probiotics: for example Enterogermina.
- Non-steroidal analgesics: they are not always recommended because they can induce constipation, delay the onset of symptoms and therapy:
- Ketorolac (for example Girolac, Rikedol, Benketol, Kevindol).
- Opioids.
- If present, prevent and treat constipation.