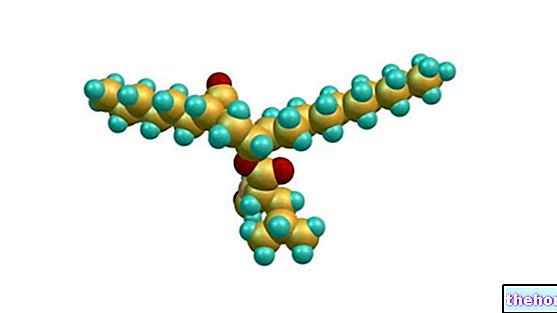
In chemistry, on the other hand, lactose is considered a small carbohydrate polymer of the disaccharide type formed by two units or monomers of the monosaccharide type, namely D-glucose and D-galactose.

This category, which also includes sucrose and maltose, groups together the smallest structures of the largest set of oligosaccharides (max 10 units).
Given the simplicity of its molecular structure and the high solubility in water that characterize it, lactose is often defined as a "simple carbohydrate" - a circle which includes the individual monosaccharides that compose it and fructose.
The chemical bond between glucose and galactose, intrinsic to lactose, is of the O-glycosidic type (β 1−4). The synthesis occurs by condensation while lysis by hydrolysis; both require a catalytic agent which, in the organism, is physiologically constituted by an enzyme.
) of each glycide: 3.75 per gram (g) - many simplify by rounding to 4.0 kcal / g.
To be sure, the function of lactose should be differentiated between glucose and galactose. The first is used almost exclusively for energy purposes, but the second constitutes some complex polymers present in the organism.
That said, although most of it comes from exogenous sources, galactose can be produced independently by the body.
Since fairly modest levels are required, the excess of galactose supplied with food acquires a caloric role comparable to that of other carbohydrates; this requires, however, its conversion into glucose by the liver.
, lactose is digested and absorbed in the small intestine.Its digestion is accomplished by a single enzyme called lactase.
This biological catalyst, positioned on the brush border of the enterocytes (intestinal mucosa cells), is responsible for the hydrolysis of the chemical bond of the disaccharide.
Only after this cleavage will it be possible to absorb glucose and galactose (by means of active transport) before the tract of the small intestine ends and that of the large intestine begins.
Lactose intolerance is the lack or insufficiency of the lactase enzyme that generates, as a consequence, adverse reactions of a typically gastrointestinal nature - even if there is no lack of related atypical symptoms.
It is a pathological condition if present in the infant, given the "essential" role of this sugar for the child's survival until weaning, and para-physiological or even physiological in post-weaning and beyond.
Note: Lactose intolerance is not an allergy (like milk protein), because the immune system is not involved in the manner typical of these conditions.
Causes of lactose intolerance
The only known cause of lactose intolerance is lactase insufficiency. However, this phenomenon can have different etiologies.
There are subjects who are born without or deficient in lactase, and in this case we speak of a genetic or primary or permanent deficit, and people who lose it, and in this case we speak of an acquired or secondary deficit.
Furthermore, the secondary or acquired lack of lactase can also be transient.
As the name suggests, the genetic deficiency is due to the inability of intestinal enterocytes to produce the enzyme for inherent causes. Conversely, the acquired deficit is often the result of one or more predisposing factors.
Among these would be mainly involved:
- lack of long-term lactose intake;
- intestinal resection;
- celiac disease;
- chronic inflammatory and autoimmune diseases;
- infectious diseases of the intestine (viral and bacterial).
It is therefore understandable that some of these causes can be treated, while others less or not at all.
Who Affects Lactose Intolerance?
Some population groups are more prone to lactose intolerance than others.
We are talking about differences related to ethnicity, heredity and predisposing pathological conditions.
For example, Asians are more prone to intolerance than Central European Caucasians, as well as there is a correlation between this condition and celiac disease and, of course, a fair familiarity is observed.
Consequences of lactose intake in intolerant people
In conditions of lactase deficiency, eating foods with lactose creates a condition that favors the onset of unwanted gastrointestinal reactions.
The mechanisms involved are mainly two: the locally toxic-osmotic action of lactose and the subsequent intervention of the intestinal physiological flora.
The result is the liquefaction of the intraluminal content, due to the recall of water in the small intestine, and a conspicuous bacterial metabolism in the large intestine with high gas production.
Clinical symptoms and signs of lactose intolerance
Symptoms and clinical signs typical of lactose intolerance are: feeling of indigestion, diarrhea, abdominal cramps, bloating and flatulence, abdominal distension; vomiting occurs with a certain frequency.
They are atypical: headaches, skin manifestations and urinary system discomfort.
The appearance of symptoms and clinical signs due to the introduction of lactose by the intolerant is rather subjective.
Obviously, the greater the lactase deficiency, the more intense the unwanted reaction should be. Mostly this is the case, but not always.
In fact, there are (infrequent) cases of subjects normally provided with lactase who in any case show the typical profile of the intolerant and, vice versa, people with little lactase who do not complain of significant severity.
Attention! If you drink warm milk, you can have similar symptoms even if you have normal lactase concentrations. This is due to the momentary conversion of lactose into lactulose, by heat, which becoming indigestible causes quite similar consequences.
How is lactose intolerance diagnosed?
Mainly with the breath-test or breath test, a non-invasive test that consists in measuring the exhaled breath - in particular of the hydrogen - after taking a load of lactose.
As previously mentioned, the availability of lactose in the colon gives the bacterial flora the ability to feed abundantly.
The waste substances include many gases, some of which do not have time to be expelled with flatulence, consequently being absorbed by the intestine and put into the bloodstream.
At this point the only way of elimination is the lung exhalation. This is why by measuring this parameter it is possible to understand the extent of intestinal fermentation of lactose and, consequently, the lack of lactase expression in the small intestine.
Treatments for lactose intolerance
The only effective treatment for lactose intolerance is its exclusion from the diet.
This can be done by removing milk, derivatives and food additives that contain the disaccharide, or by replacing them with delactosed foods (in which lactose is broken down into glucose and galactose). However, scientific research and the food industry did not stop there.
There are products based on lactase enzymes to be taken by mouth that should replace the physiological role of enterocytes. The results are however controversial and to date it is not possible to consider them a valid therapeutic solution in the chronic for all lactose intolerant subjects.
and the like, ricotta, cheeses, etc.) have chemical characteristics that are anything but negligible.Milk, yogurt and the like, ricotta, cheese are excellent nutritional sources of high biological value proteins (essential amino acids), vitamin B2 (riboflavin), calcium and phosphorus.
, milk cream, ricotta, emmenthal, mozzarella etc.
Foods that contain powdered additives derived from milk should not be underestimated. These, with an absorbent and preservative function, are used above all in the production of ground sausages such as salami.