" introduction
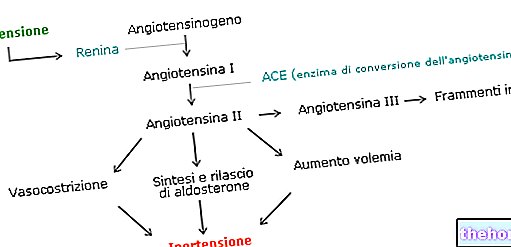
As anticipated, the entire renin-angiotensin system is primarily regulated at the renal level. The passage of renin into the circulation is in fact stimulated by all those factors that determine hypotension, such as hypovolemia, sodium depletion, vasodilation and factors that favor it (glucagon, bradykinin, PGE2, PGE1). On the other hand, the passage of renin into the circulation, and with it the hypertensive effects of angiotensin II, are inhibited by "hypervolemia, by" hypertension, by sodium retention, by vasoconstriction and by the factors that favor (mineralocorticoids, vasopressin-diuretic, which also induces hypervolemia by promoting water reabsorption in the kidney). Finally, there is a negative feed-back control whereby the production of renin is inhibited by its own product, which is precisely angiotensin II.

The regulation of the renin angiotensin system is also heavily influenced by the activity of the ACE, since the angiotensin I generated by the proteolytic cut of the renin sharply increases its activity only after being transformed into angiotensin II by the aforementioned enzyme. conversion This enzyme is particularly expressed at the level of the pulmonary vascular endothelium; very importantly, it also acts on bradykinin (which has a vasodilatory action), transforming it into inactive products. The tissues of the organism, however, are not a simple "target" of angiotensin, but are themselves capable of producing it locally through various enzymes. Beyond the actions described so far and known for some time, in recent years the attention of researchers has been focusing on the tissue renin-angiotensin system (SRA), involved in events such as the formation of atheromatous plaques and proliferative phenomena of the walls vascular.
In many people the circulating and tissue renin-angiotensin system is excessive or abnormal, to the point of playing a pathological role essentially characterized by hypertension. In these cases, the so-called ACE inhibitor drugs are used, which reduce the synthesis of angiotensin II and aldosterone, rebalancing blood pressure. Other newer medicines, sartans, have the same effect by blocking the AT1 receptors of angiotensin.
In addition to promoting the contraction of smooth muscle cells, angiotensin - if chronically produced to an excessive extent - also stimulates hyperplasia. ACE inhibitors are therefore used in the treatment of diabetic micro and macroangiopathy, thanks also to their vasodilatory effect mediated by the inhibition on the degradation of bradykinin (which leads to an increase in the production of nitric oxide and other vasoactive substances, such as EDFH, with antiplatelet and antiproliferative effect). The increase in bradykinin and other kinins, however, also determines some typical side effects of these drugs, such as dry cough and angioedema. These drugs are also used in the treatment of post-heart attacks, chronic heart failure (they reduce blood pressure and myocardial hypertrophy, and positively influence ventricular remodeling after myocardial infarction) and diabetic nephropathy; also probable an antithrombotic-antiatherogenic effect and consequent usefulness in the secondary prevention of ischemic heart disease Sartans, on the other hand, do not inhibit the degradation of bradykinin and other kinins, and therefore have fewer side effects.