Normal development of red blood cells
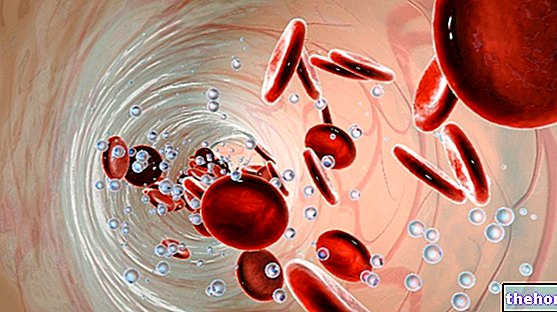
The development of blood cells is called hematopoiesis, while the specific development of red blood cells or erythrocytes is called erythropiesis.
The bone marrow, lymph nodes and spleen are all organs involved in hematopoiesis. Traditionally they are distinguished:
- a myeloid tissue, including the bone marrow and the cells that originate from it: red blood cells, platelets and granulocyte-monocytes (white blood cells).
- a lymphoid tissue, consisting of thymus, lymph nodes, spleen and the cells that originate from them: the B and T lymphocytes.
The mature elements of the blood all originate from a single hematopoietic stem cell, called multipotent because it represents the common precursor from which all blood cells can derive without distinction. From it subsequently develop lymphoid stem cells (which will give life to lymphocytes) and myeloid stem cells relating to the three medullary lines (erythrocytes, granulocytes - monocytes and platelets), destined respectively for the production of lymphocytes and myeloid cells.

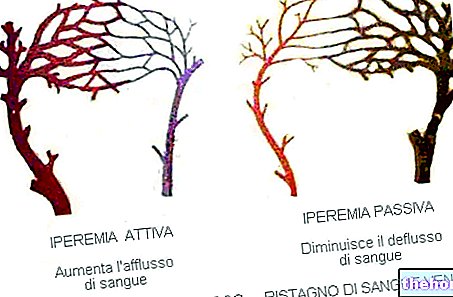
The stem cells commissioned from the erythroid lineage are the first progenitors sensitive to erythropoietin (Epo), a protein produced by the kidney, whose action is essential for the development and maturation of red blood cells.
The kidney cells are equipped with an oxygen quantity sensor and, according to the degree of hypoxia (reduction of oxygen) of the blood supplying them, regulate the secretion of erythropoietin. This hormone, by binding to a receptor of erythroid cells, determines in them a response that consists in the increase of their division, of the synthesis of hemoglobin (the iron-protein that is contained in red blood cells and that binds oxygen) and of the receptors for transferrin (the protein that binds iron and transports it into the bloodstream).
The mature red blood cell, to become such, must follow some maturation stages:
- Proerythroblast
- Basophil Erythroblast
- Polychromatophilic Erythroblast: begins to synthesize Hemoglobin
- Erythroblast Orthochromatic: expels the nucleus contained within it (red blood cells are cells without a nucleus!)
- Reticulocyte: leaves the bone marrow and enters the bloodstream
- Mature erythrocyte.
Structure of the erythrocyte
The red blood cell is a cell with an outer membrane and cytoplasm, but without a nucleus and cytoplasmic organelles. The completely differentiated erythrocyte, in practice, is formed only by a plasma membrane that encloses hemoglobin and a limited number of enzymes, necessary for maintaining the integrity of the membrane and for the function of transporting gases. Its color is pink, due to its high hemoglobin content, which is basic, that is, it binds acid dyes which are themselves pink.
Its shape is a "biconcave disc"; this determines a larger surface area than the spherical shape, and this allows to significantly increase the gaseous exchanges.
The fluidity of the membrane allows the erythrocyte to deform easily, so that it can pass even through the smallest capillaries.
Hemoglobin is a protein made up of four polypeptide chains (of many amino acids) that are two by two equal: two alpha chains and two beta chains. Each chain binds a heme radical, which is a structure capable of binding an iron molecule Thus a hemoglobin molecule, which contains four heme radicals, is capable of binding four iron molecules. Iron binds oxygen; from this we deduce that hemoglobin is a protein capable of binding oxygen and transferring it to the tissues in physiological conditions, according to their needs.
Function of red blood cells
Red blood cells have a main function which is to carry oxygen to the tissues.The appearance (morphology) assumed by the erythrocytes upon examination of the peripheral blood smear (blood is taken from the subject, smeared on a slide and looked at the optical microscope) is of great importance:
The size of the erythrocytes: normocytes (normal size), microcytes (decrease), macrocytes (increased)
The degree of hemoglobinization, which is reflected in the color of the erythrocytes: normochromic or hypochromic (clearer).
The shape of the erythrocytes
These values are also measured objectively and are called erythrocyte indices. In most laboratories there are instruments that measure them directly or calculate them automatically. They are:
MCV or Average corpuscular volume: is the volume of a red blood cell, expressed in fentoliters (cubic micrometers). Normal values are considered to be those between 80 and 95 fentoliters. An "anemia is called microcytic when MCV is lower than the normal range and macrocytic when MCV is higher.
MCH or Mean corpuscular hemoglobin: is the average content (mass) of hemoglobin per red blood cell, expressed in picograms. Normal values are between 27 and 33 picograms.
MCHC or Mean corpuscular concentration of hemoglobin: is the average concentration of hemoglobin in a given volume of sedimented red blood cells, and is expressed in grams per deciliter. Normal values are between 33 and 35 grams per deciliter.
RDW or Distribution width of red blood cells: is the variation coefficient of the erythrocyte volume. Normally it is between 11% and 14%.
Reference values
Normal average red blood cell values vary by sex, but also by age
Therefore also the normal ranges adopted by the various analysis laboratories may vary. As an indication, the following normal ranges can be taken as a reference
- adult males: 4.5-6 million / mm3 (4,500,000-6,000,000 / mm3)
- adult women: 4-5.5 million / mm3 (4,000,000-5,500,000 / mm3)
DID YOU KNOW THAT: The different concentration of red blood cells and hemoglobin in the two sexes is due to the greater presence of testosterone in the male organism. This powerful anabolic hormone in fact stimulates erythropoiesis, ie the formation of new red blood cells.