Key points
Definition of hyponatremia
Sodium concentration in the blood
Classification and causes of hyponatremia
- Hypertonic hyponatremia: caused by hyperglycemia
- Isotonic hyponatremia or pseudohyponatremia: caused by the exaggerated increase in lipids and / or plasma proteins
- Hypotonic hyponatremia: caused by the "increase in" the hormone ADH → water retention → hyponatremia
- Hypervolemic hyponatremia: caused by congestive heart failure, liver failure, cirrhosis, kidney disease
- Euvolemic hyponatremia: caused by syndrome of inappropriate hypersecretion of antidiuretic hormone (SIADH), hypothyroidism, adrenal insufficiency, polydipsia
- Hyponatremia hypovolaemia: caused by taking diuretics, renal loss of salts, mineralocorticoid deficiency, diarrhea, vomiting, severe burns, pancreatitis, trauma
Symptoms of hyponatremia
Hallucinations, Ascites, Convulsions, Muscle cramps, Epilepsy, Hypotension, Headache, Loss of consciousness, Dry mouth, Intense thirst, Severe somnolence, Tachycardia
Therapies for hyponatremia
- Water restriction
- Intravenous hypertonic saline solutions
- Hormone therapy (for Addison's disease-dependent forms)
- Tolvaptan
- Demeclocycline or lithium
Definition of hyponatremia
We speak of hyponatremia - or hyponatremia - when the concentration of sodium in the blood (sodemia) is abnormally low (serum sodium does not meet the needs of the body.
As we know, sodium is a very important electrolyte, also useful for regulating the amount of intra / extra cellular water.
To understand...
Sodium represents the main electrolyte of the extracellular fluid: 90% of the total body sodium is contained in the extracellular compartment, thanks to the action of the enzyme Na + - K + ATPase (which actively transports sodium out of the cell).

Sodium is also involved in the transmission of nerve impulses, in cellular exchange and in muscle contraction: according to this, we understand how a condition of hyponatremia can upset all these functions which the body must perform.
Sodemia expresses the concentration of sodium in the blood, and is expressed in mmol / L
Although the daily water intake is extremely variable, the serum sodium concentration fluctuates in a very narrow range (135-145 mmol / L), thanks to the extraordinary ability of the kidney to dilute or concentrate urine.
We speak of hyponatremia proper when the serum sodium concentration falls below the value of 135mmol / L. The finding of hyponatremia - very frequent in sports - can also accompany dysmetabolic diseases (diabetes, hyperglycemic coma, etc.).
Causes
It is not always so immediate to trace the pathophysiological mechanisms underlying the electrolyte imbalance. In general, hyponatremia is favored by a LOSS OF SODIUM or by a severe WATER RETENTION.
The etiopathological factors most involved in hyponatremia are:
- Intake of excessive amounts of water
- Extensive burns
- Liver cirrhosis *
- Low sodium diet
- Severe and prolonged diarrhea
- Intense physical exercise for a long time → excessive sweating
- Diuretic, antidepressant, antitumor drugs
- Congestive heart failure *
- hypothyroidism
- Addison's disease
- Renal pathologies
- Syndrome of inappropriate antidiuretic hormone secretion (SIADH): ↑↑ vasopressin (antidiuretic hormone) → ↓ emission, storage of water in the blood and increased volume → dilution of electrolytes in the blood → ↓ sodium
- Sweating
- Drug addiction (especially ecstasy)
- Brain trauma and severe burns
- He retched
* Hyponatremia is believed to predict death among patients with cirrhosis or congestive heart failure:
1. hyponatremia due to heart failure → ↓ cardiac output and ↓ blood pressure → ↑↑ secretion of "hypovolemic" hormones renin, ADH, aldosterone → water and sodium retention in the kidney, increased blood volume with sodium dilution and inability to eliminate "water taken
2. hyponatremia due to liver cirrhosis → ↓ protein synthesis → reduction of oncotic blood pressure → appearance of edema and hypovolemia → ↑↑ secretion of "hypovolemic" hormones renin, ADH, aldosterone → water and sodium retention in the kidney, increase in volume with sodium dilution and inability to eliminate the water taken
Although it is still essential to weigh the intake of excessively salty foods, it is clear that the complete removal of salt from the diet is not a very sensible and intelligent attitude. Just think of the risks that an athlete can run following a similar behavior: the loss of salts during sport must be restored by taking isotonic drinks. Otherwise - for example by taking the famous "low sodium" waters afterwards intense physical exertion - the risk of hyponatremia is raised, as the blood sodium already reduced by profuse sweating is further diluted.
Classification
After having listed the possible triggering causes of hyponatremia, we distinguish three variants:
- HYPER-OSMOLAR HYPONATREMIA [osmolarity> 296 mOsm / kg H2O]: rather rare, it is essentially caused by the perfusion of hypertonic liquids, therefore too rich in solutes (eg mannitol, sorbitol, maltose, glucose or intravenous infusion of immunoglobulins). Hyperosmolar hyponatremia is often linked to hyperglycemia.
- PSEUDOIPONATREMIA or ISOTONIC HYPONATRIEMIA [osmolarity 280-296 mOsm / kg H2O]: the (apparent) reduction of sodaemia is a consequence of an exaggerated increase in lipids and / or plasma proteins
- HYPO-OSMOLAR HYPONATREMIA [osmolarity <280 mOsm / kg H2O]: it is an expression of the kidney's inability to eliminate a sufficient quantity of free water compared to that assumed.
- Hypotonic or hypovolemic dehydration → hyponatremia associated with VOLEMIC DEPLETION (reduction). Clinical condition caused by taking diuretics, renal loss of salts, mineralocorticoid deficiency (sodium> 20 mmol / L) or by diarrhea, vomiting, severe burns, pancreatitis, trauma (sodium
- Hypotonic hyperhydration or dilution hyponatremia or Hypervolemic hyponatremia → hyponatremia WITH EDEMA: cirrhosis, nephrotic syndrome, heart / renal failure
- Isovolemic or euvolemic hyponatremia: absence of edema and volume depletion. Characteristic condition of water intoxication, hypothyroidism, SIADH, glucocorticoid deficiency and primary polydipsia (intense thirst)
In the next article, the symptoms, diagnostic strategies and treatments currently available for the treatment of hyponatremia are analyzed.
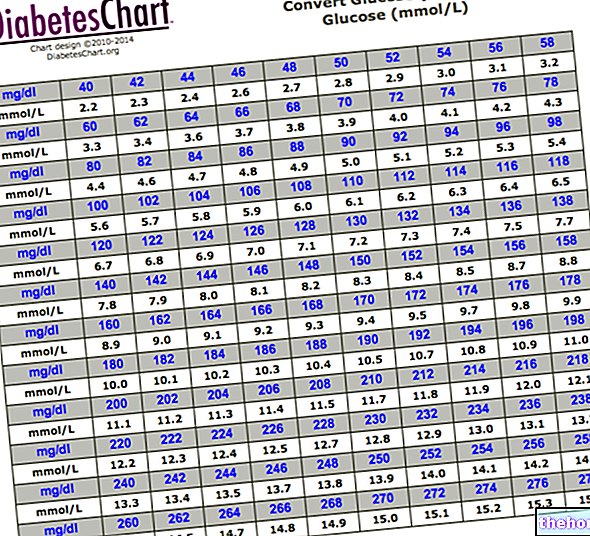
Select Blood Tests Blood Tests Uric acid - uricaemia ACTH: adrenocortitotropic hormone Alanine amino transferase, ALT, SGPT Albumin Alcoholism Alphafetoprotein Alphafetoprotein in pregnancy Aldolase Amylase Ammonemia, ammonia in the blood Androstenedione Antibody-endomysial antibodies Anti-gliadicides Nucleus Helicobacter pylori antibodies Embryo carcinoal antigen - CEA Prostate specific antigen PSA Antithrombin III Haptoglobin AST - GOT or aspartate aminotransferase Azotemia Bilirubin (physiology) Direct, indirect and total bilirubin CA 125: tumor antigen 125 CA 15-3: tumor antigen 19-9 as tumor marker Calcemia Ceruloplasmin Cystatin C CK-MB - Creatine kinase MB Cholesterolemia Cholinesterase (pseudcholinesterase) Plasma concentration Creatine kinase Creatinine Creatinine Creatinine clearance Chromogranin A D-dimer Hematocrit Blood culture Hemocrome Hemoglobin Glycated hemoglobin a Blood tests Blood tests, Down syndrome screening Ferritin Rheumatoid factor Fibrin and its degradation products Fibrinogen Leukocyte formula Alkaline phosphatase (ALP) Fructosamine and glycated hemoglobin GGT - Gamma-gt Gastrinemia GCT Glycemia Red blood cells Granulocytes HE4 and Cancer at "Ova" Immunoglobulins INR Insulinemia Lactate dehydrogenase LDH Leukocytes - white blood cells Lymphocytes Lipases Tissue damage markers MCH MCHC MCV Metanephrines MPO - Myeloperoxidase Myoglobin Monocytes MPV - average platelet volume Natremia Neutrophils Homocysteine Thyroid hormones OGTT Osmocyte Plasma protein A associated with pregnancy Peptide C Pepsin and pepsinogen PCT - platelet or platelet hematocrit PDW - distribution width of platelet volumes Platelets Plateletpenia PLT - number of platelets in blood Preparation for blood tests Prist Test Total IgEk Protein C (PC) - Protein C Activated (PCA) C Reactive Protein Rast Protein Test Specific IgE Reticulocytes Renin Reuma-Test Oxygen Saturation Sideremia BAC, BAC TBG - Thyroxine Binding Globulin Prothrombin Time Partial Thromblopastin Time (PTT) Activated Partial Thromboplastin Time (aPTT) Testosterone Testosterone: free and bioavailable fraction Thyroglobulin Thyroxine in the blood - Total T4, free T4 Transaminases High transaminases Transglutaminase Transferrin - TIBC - TIBC - UIBC - saturation of transferrin Transtyretin Triglyceridemia Triiodothyronine in the blood - Total T3, free T3 Troponin TRH and Troponins of s thymol to TRH TSH - Thyrotropin Uremia Liver values ESR VDRL and TPHA: serological tests for syphlis Volemia Conversion of bilirubin from mg / dL to µmol / L Conversion of cholesterol and triglyceridemia from mg / dL to mmol / L Conversion of creatinine from mg / dL to µmol / L Conversion of blood glucose from mg / dL to mmol / L Conversion of testosteronemia from ng / dL - nmol / L Conversion of uricemia from mg / dL to mmol / L














.jpg)











