The term alveolus derives from the Latin alveolus → small cavity.
Despite their small size, the pulmonary alveoli are responsible for a very important function: the exchange of respiratory gases between the blood and the atmosphere.

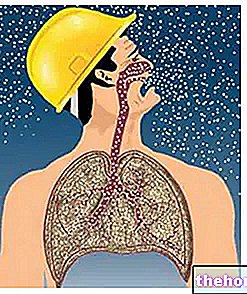
Most of the pulmonary alveoli gather in groups located at the extremity of each respiratory bronchiole. Through the latter they receive the atmospheric air coming from the contiguous upper tracts of the airways (terminal bronchioles, bronchioles, tertiary, secondary and primary bronchi, trachea , larynx, pharynx, nasopharynx and nasal cavity).
Hemispheric protrusions, called pulmonary alveoli, begin to be recognized along the wall of the respiratory bronchioles.
The respiratory bronchioles preserve the branched structure of the bronchial tree, increasing the number of alveoli housed as they originate ducts of a lower caliber.

The pulmonary alveoli appear as small air chambers of spherical or hexagonal size, with an average diameter of 250-300 micrometers in the phase of maximum insufflation. The primary role of the alveoli is to enrich the blood with oxygen and clean it of carbon dioxide. The high density of these alveoli characterizes the spongy morphological aspect of the lung; in addition, the gas exchange surface significantly increases, which overall reaches 70 - 140 square meters in relation to sex, age, height and physical training (we are talking about an "area equal to an apartment with two rooms or a tennis).
The wall of the alveoli is very thin and consists of a single layer of epithelial cells. Unlike the broncholes, the thin alveolar walls are devoid of muscle tissue (because it would hinder gas exchange).Despite the impossibility of contracting, the abundant presence of elastic fibers gives the alveoli a certain ease in extension during the inspiratory process and elastic return during the expiratory phase.
The region between two adjacent alveoli is known as the interalveolar septum and consists of alveolar epithelium (with its 1st and 2nd type cells), alveolar capillaries and often a layer of connective tissue. The intralveolar septae strengthen the alveolar ducts and somehow stabilize them.
The pulmonary alveoli can be connected to other adjacent alveoli via very small holes, known as pores of Khor. The physiological significance of these pores is probably to balance the air pressure within the lung segments.
The pulmonary acinus represents the territory of the parenchyma dependent on a terminal bronchiole. The pulmonary acini represent the last portions of the pulmonary lobule. The pulmonary lobules constitute the broncho-pulmonary areas. The broncho-pulmonary areas constitute the pulmonary lobes ( three in the right lung, two in the left).
Structure of the alveoli
Each pulmonary alveolus consists of a single and thin layer of exchange epithelium, in which two types of epithelial cells are known, called pneumocytes:
- Squamous alveolar cells, also known as type I cells or respiratory epitheliocytes;
- Type II cells, also known as septal cells or surfactant cells;
Most of the alveolar epithelium is formed by type I cells, which are arranged to form a continuous cell layer. The morphology of these cells is very particular, because they are very thin and have a small swelling at the nucleus, where they they accumulate the various organelles.

The alveolar epithelium is also composed of type II cells, scattered singly or in groups of 2-3 units among the type I cells. The septal cells have two main functions. The first is to secrete a liquid rich in phospholipids and proteins , called surfactant; the second is to repair the alveolar epithelium when it is seriously damaged.
The surfactant liquid, continuously secreted by the septal cells, is able to prevent excessive distension and collapse of the alveoli. Furthermore, it helps to facilitate the exchange of gas between the alveolar air and the blood.
Without the production of surfactant by type II cells, serious respiratory problems, such as total or partial collapse of the lung (atelectassia), would develop. This condition can also be caused by other factors, such as trauma (pneumothorax), pleurisy or chronic obstructive pulmonary disease (COPD).
Type II alveolar cells appear to help minimize the volume of liquid present in the alveoli, by conveying water and solutes out of the air spaces.
The presence of immune cells is recorded in the pulmonary alveoli. In particular, the alveolar macrophages are responsible for the elimination of all those potentially harmful substances, such as atmospheric dust, bacteria and polluting particles. Not surprisingly, these monocyte derivatives are known as dust or dust cells.
Blood circulation
Each pulmonary alveolus has a "high vascularization, guaranteed by numerous capillaries. Inside the pulmonary alveoli, the blood is separated from the" air by a very thin membrane.

The oxygen-rich blood from the pulmonary veins reaches the left ventricle of the heart. Then, thanks to the activity of the myocardium, it is pushed into all parts of our body. The blood to be "cleaned", on the other hand, starts from the right ventricle and reaches the lungs through the pulmonary arteries. pulmonary veins carry oxygenated blood while arteries carry venous blood, the exact opposite of what has been seen for the systemic circulation.
In a person at rest, the quantity of oxygen exchanged between the alveolar air and the blood is around 250-300 ml per minute, while the quantity of carbon dioxide diffused from the blood to the alveolar air is around 200-250 ml. . These values can increase by about 20 times during an intense "sporting activity.


.jpg)