Generality
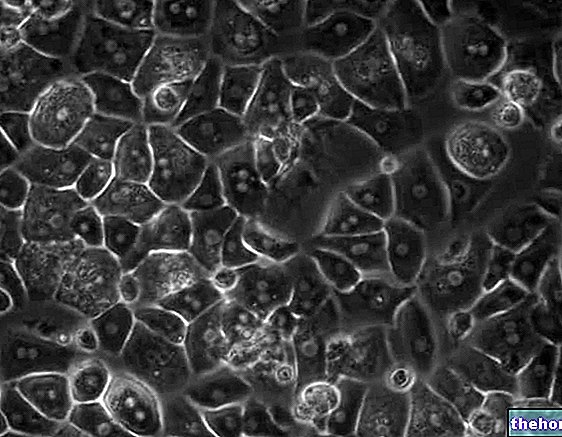
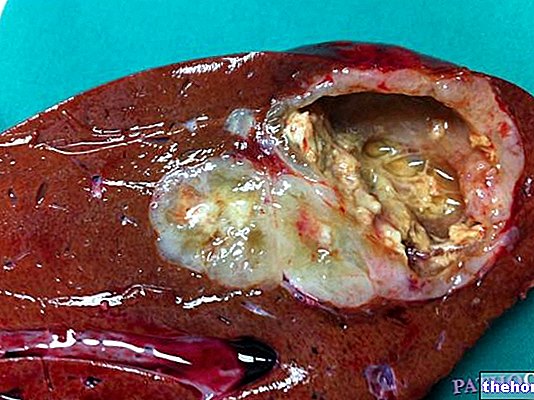
Liver biopsy is a medical procedure based on the removal of a fragment of liver tissue using a dedicated needle, with the ultimate aim of studying it under a microscope to identify and characterize various liver diseases. The liver biopsy can therefore be used as a diagnostic tool in the presence of suspicion of a liver disease that cannot be investigated with other techniques, or as a tool to establish its severity if it has already been ascertained in other ways. The information provided by a positive liver biopsy also makes it possible to formulate a prognosis and to analyze the most suitable therapeutic intervention possibilities.
Main indications
Since it is an invasive and therefore potentially dangerous examination, liver biopsy should only be performed when the patient can derive tangible clinical benefits, or when it is not possible to obtain adequate diagnostic information with less invasive or non-invasive methods.
The main indications for liver biopsy include the diagnosis, staging and grading (stage and grade) of alcoholic liver disease, non-alcoholic steatohepatitis (complications of the so-called fatty liver), autoimmune hepatitis and chronic viral hepatitis of type B and C.

How it is done
Based on clinical needs, liver biopsy can be performed using several techniques:
- sampling during surgery;
- biopsy during laparoscopic investigation;
- transjugular biopsy;
- percutaneous biopsy (covered);
- ultrasound-guided percutaneous biopsy on focal lesion.
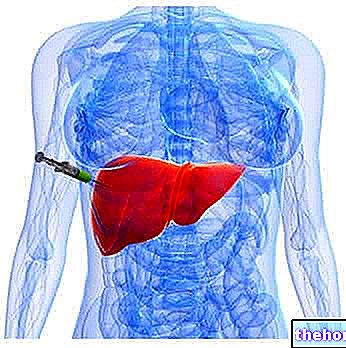
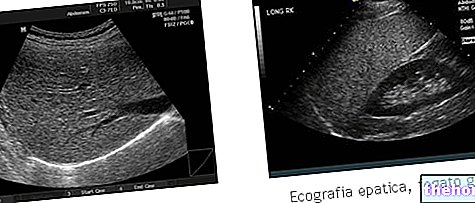
Among these, the most common is undoubtedly percutaneous liver biopsy (ultrasound-guided or not). During the examination, the patient lies supine or more commonly on the left side, with the right arm placed behind the head. The adoption of this particular position, however comfortable, aims to increase the space between the ribs. With the help of ultrasound the doctor identifies the liver and the body region most suitable for puncture, disinfects it and injects a local anesthetic. At this point, a larger biopsy needle (diameter of about 1.2 mm) is introduced and rapidly withdrawn into the patient's liver, collecting a small piece of liver tissue. The operation does not last more than a couple of seconds and requires the patient's active cooperation. In fact, before the "introduction of the" needle, he is invited to exhale deeply (letting all the air out of the lungs) and to hold his breath (apnea) for a few seconds, sufficient to insert and withdraw the biopsy needle. This is particularly useful, since the airless lungs are smaller and the liver is higher in the abdomen.
In the rare event that not enough tissue has been removed, the maneuver will have to be repeated a second time.
In addition to the local anesthetic, at the discretion of the doctor, a mild sedative (benzodiazepine) and / or intramuscular atropine can be administered; this allows to promote the state of relaxation without impeding the important active collaboration of the patient, at the same time preventing any alterations blood pressure and heart rate.
The procedure described above is also defined as eco-assisted, since the correct puncture site is established by means of an ultrasound examination. A variant, called percutaneous ultrasound-guided biopsy on focal lesion, provides instead a constant ultrasound monitoring. The purpose of this procedure is in fact to take cellular samples of hepatic tissue from a specific region of the liver (focal lesion), for example in the "area where" an abnormal formation was found.
As anticipated, the liver biopsy can also be performed during a major surgery (under general anesthesia) or minimally invasive laparoscopically, ie through the insertion - through one or more small incisions of the skin and muscle groups - of small instruments , including a micro-camera for direct vision sampling. Laparoscopic liver biopsy can be performed when there is a danger of spreading infection or cancer cells.
Transjugular biopsy is a complex method used in patients forced to take chronic anticoagulant therapies, with hemorrhagic diseases or with ascites. The method involves the insertion of a cannula into a vein in the neck, which is then made to go down to the hepatic veins for sampling.
In the following paragraphs we will analyze the risks, complications and operating methods of percutaneous liver biopsy alone, which we remember to be the most commonly used technique.
Liver biopsy: risks and preparation "