Diabetes is not a real disease, but a set of chronic syndromes characterized above all by hyperglycemia, and due to the malfunction of the pancreatic cells responsible for the production of insulin and / or to an increase in insulin resistance by peripheral tissues ( muscle, adipose and hepatic tissues).
Insulin secretion occurs in the endocrine pancreas and is entrusted to the β cells of the islets of Langerhans. Other important hormones are also secreted in the pancreas, such as glucagon from α cells, somatostatin from δ cells and pancreatic polypeptide from PP cells; these hormones self-control each other by also regulating the release of insulin.
The synthesis of insulin follows a multi-step path; first the pre-insulin precursor is secreted by the β cells into the rough endoplasmic reticulum; after which, the pre-insulin - consisting of three polypptide chains A, B and C - is first transformed into pro-insulin at the level of the Golgi apparatus, by endopeptidases that detach the C unit, and finally into insulin (chain polypeptide A linked by disulfide bridges to the polypeptide chain B) associated with peptide G.
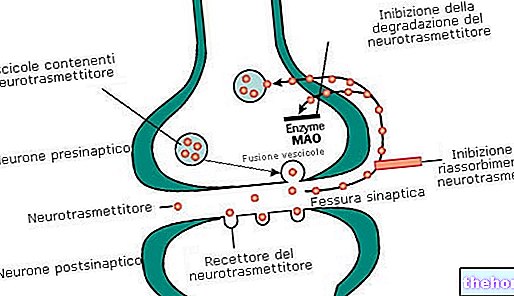
Insulin secretion is regulated: by the ortho and parasympathetic neurovegetative system, respectively, the ortho stimulates secretion and para inhibits it, from nutritional principles, from pancreatic hormones, respectively, somatostatin inhibits and glucagon stimulates, and from gastrointestinal hormones Generally we tend to say that the secretion of insulin is regulated by the levels of blood sugar, in fact all the nutrients, carbohydrates, lipids and proteins are able to raise the blood sugar, therefore to influence the secretion of insulin.
The main function of insulin is to keep the concentration of glucose in the blood constant, through various metabolic devices: the transformation of glucose into glycogen (energy reserve) in the liver, the deposit of excess glucose into triglycerides in the adipose tissue; the increase in the peripheral uptake of glucose by cells for energy purposes; the increase in the uptake of amino acids at the cellular level, especially in the muscles, where they are channeled into the production of proteins. When insulin secretion is inhibited, the degradation of glycogen, proteins and triglycerides is favored to release simple glucose, free amino acids and fatty acids. The importance of insulin lies precisely in its regulatory properties on energy sources; these are accumulated in the form of reserves, if in excess, or are consumed when necessary.
Insulin performs its function by interacting with the metabotropic tyrosine kinase receptor. This is a monomer that crosses the cell membrane with an "external end that acts as a binding site, and an" intracellular end that exhibits the kinase function. Phosphorylation cross of two receptor monomers allows the activation of both receptors and the subsequent phosphorylation reactions, which lead to all the metabolic reactions listed above, characterized by their slow evolution.
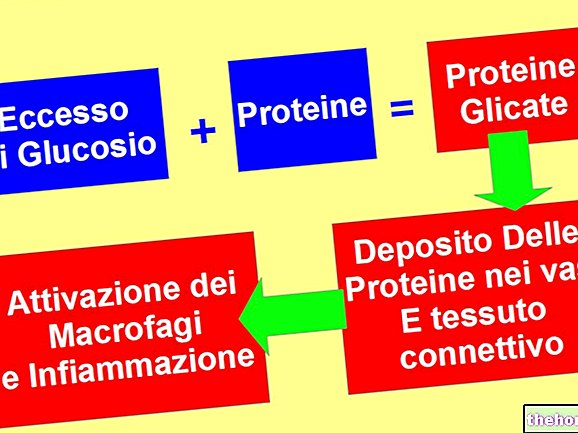
Diabetes, therefore, not only alters blood sugar, but also the metabolism of proteins and lipids; moreover, diabetes increases the risk of onset of cardio-vascular diseases, especially retinopathies, glomerulopathies and neuropathies, due to a thickening of the vascular wall and insufficient blood circulation.
Diabetes is a widespread disease, especially in the so-called welfare countries, where some risk factors, such as obesity and a sedentary lifestyle, favor its onset. Diabetes can be distinguished into different types of syndromes; the most important are:
- the primary or spontaneous diabetes it represents the most common, in turn it is divided into type 1 diabetes and type 2 diabetes;
- the secondary diabetes, resulting from diseases related to the pancreas or intense pharmacological treatments based on glucocorticoids;
- pregnancy diabetes.
Type 1 diabetes or insulin-dependent diabetes characterizes patients with total insulin deficiency and completely degenerated β cells. Sometimes it can be caused by incorrect autoimmune responses against the β cells of the pancreas, or more commonly it is triggered by the presence of obesity, environmental and hereditary factors; in this case it is called idiopathic diabetes. This type of diabetes arises very early, even during childhood. Insulin-based therapy is unique and cannot be eliminated for the entire life span.
Type 2 diabetes or insulin-independent diabetes, on the other hand, characterizes patients who retain a certain functionality of β cells (although not sufficient to maintain stable blood glucose levels), but have a poor sensitivity of peripheral tissues to insulin. typology is not immune, but multifactorial, based on behavioral, hereditary and environmental elements.Unlike the first type, this form of diabetes most commonly arises in old age, therefore it is also known as senile diabetes.
The most important alterations caused by diabetes concern some important catabolic reactions, contrary to the anabolic ones mediated by insulin: hyperglycemia, caused by a reduced uptake of glucose in the periphery, by a more intense hepatic gluconeogenesis and by a reduction in glycogen reserves. ; the "increased degradation of proteins and a reduced capacity of uptake of amino acids by the cells; the" increased degradation of lipids, with consequent formation of glycerol, used as a substrate for the formation of new glucose, and fatty acids (the latter carry to the formation of ketone bodies which accumulate generating metabolic acidosis).
More articles on "Diabetes, Types of Diabetes, Causes and Consequences of Diabetes"
- Constipation: Laxatives and drugs against constipation
- Insulin in the treatment of diabetes


.jpg)