Definition
Atrial fibrillation is one of the most common forms of cardiac arrhythmia, consisting in the chaotic and fragmentary contraction of the atria, which therefore causes an irregular and often accelerated heart rhythm; it is a supraventricular tachyarrhythmia characterized by progressive damage to the atrial mechanical function. Atrial fibrillation can become chronic or appear suddenly and resolve in a few days.
Causes
Cardiac anomalies, in terms of structure and functionality, are the etiopathological elements most involved in the manifestation of atrial fibrillation; Other predisposing factors include: drug abuse, alcoholism, heart valve abnormalities, sleep apnea, heart attacks, congenital heart defects, exposure to stimulant drugs, emphysema, viral infections, heart surgery, hypertension, hyperthyroidism, excessive stress.
Symptoms
In atrial fibrillation, the heart does not pump blood efficiently; in some patients the disorder does not create any noticeable symptoms, while in others, atrial fibrillation can cause drop in blood pressure, confusion, weakness, chest pain, shortness of breath and palpitations
- Clinical evidence: in atrial fibrillation the heart rate can vary from 100 to 175 beats / min (the normal range is between 60 and 100 bpm)
The information on Atrial Fibrillation - Medicines to Treat Atrial Fibrillation is not intended to replace the direct relationship between the healthcare professional and the patient. Always consult your doctor and / or specialist before taking Atrial Fibrillation - Medicines to Treat Atrial Fibrillation.
Medicines
As with most diseases, the treatment of choice for the treatment of atrial fibrillation depends on the triggering cause: for example, when the alteration of the heartbeat depends on a pathology affecting the thyroid gland or an alteration in blood pressure, the treatment of the diseases that are at the origin also implies the control of heart rate and rhythm. In this case, atrial fibrillation is easy to resolve; unfortunately, in practice it is not always so easy to keep the heartbeat inside the normal range, for which further pharmacological and non-pharmacological treatments are necessary. Among the most validated therapeutic strategies, we remember:
- Pharmacological control of heart rate
- Prevention of complications (stroke, heart failure)
- Electrical or drug cardioversion with antiarrhythmic drugs (in order to restore sinus rhythm)
- Prevention of thrombus formation
- Cardiac catheterization (for extreme cases)
- Ablation of the atrioventricular node in association with anticoagulant therapy
The following are the classes of drugs most used in the therapy against atrial fibrillation, and some examples of pharmacological specialties; it is up to the doctor to choose the most suitable active ingredient and dosage for the patient, based on the severity of the disease, the state of health of the patient and his response to treatment:
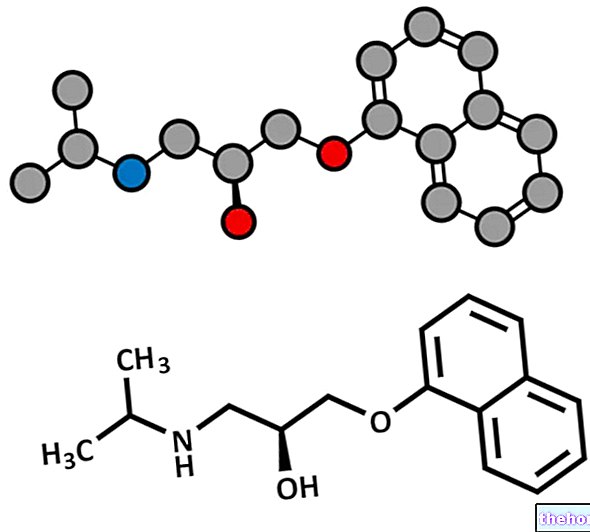
Antiarrhythmics: after electrical cardioversion to restore the physiological heartbeat, the administration of antiarrhythmic drugs is recommended to prevent further possible recurrences of atrial fibrillation episodes. These active ingredients are not without side effects (fatigue, nausea, dizziness. They can rarely cause ventricular arrhythmias): it is recommended to respect the dosage prescribed by the doctor.
- Amiodarone (eg. Cordarone, Amiodarone SAN, Amiodar, Angoron): for the treatment of atrial fibrillation, take 200 mg of the drug, three times a day for 7 days. After one week, reduce the dose to 200 mg, to be taken twice a day for 7 days. The maintenance dose involves administering 200 mg of active ingredient per day. The drug can also be administered by intravenous infusion. Consult your doctor.
- Dronedarone (eg. Multiaq): indicated for patients with a previous history of atrial fibrillation or who suffer from this disorder in a non-permanent way. Administer one 400 mg tablet orally, twice a day (preferably during breakfast and dinner). Do not take with grapefruit juice.
- Propafenone (eg Rytmonorm, Cardiofenone, Normarit): indicated for the cardioversion of atrial fibrillation, as well as for the control of the heartbeat. It is recommended to take 600 mg of the drug orally or 1.5-2mg / kg, by i.v. infusion. lasting 20 minutes. For the prevention of relapse of atrial fibrillation, take 450-900 mg per day of the drug, orally. The drug can create visual impairment, asthenia, diarrhea, nausea, dry mouth and vomiting.
- Sotalol (eg Rytmobeta, Sotalex, Sotalol TEV): for the treatment of atrial fibrillation in adults, it is recommended to take the drug orally at the indicative dosage of 80 mg, twice a day. In case the dose just described is not should bring any appreciable benefit to the patient, it is possible to increase the dosage up to 120-160 mg. Consult your doctor. The maintenance dosage involves administering the drug at a dose of 120-160 mg, orally, in double daily doses. Alternatively , it is also possible to undertake parenteral therapy: start therapy with 112.5 mg, intravenously, once or twice a day. The maintenance dose suggests taking 112.5-150 mg, intravenously, one or two times a day. The drug can also be taken by children suffering from atrial fibrillation, at a different dosage, established by the doctor based on the age, weight of the child and the severity of the disease.
- Dofetilide (eg Tikosyn): powerful third class antiarrhythmic drug, used both in the treatment of tachycardia and for the treatment of atrial fibrillation. The indicative dose is to take 125-500 mcg of active ingredient once or twice a day. The precise dose must be determined by the doctor.
- Flecainide (eg Almarytm, Flecainide SAN): start therapy with a drug dose of 100 mg, to be taken by mouth every 12 hours. The maintenance dose may increase by 50 mg every 4 days from the starting dose. Do not exceed 400 mg per day.
- Vernakalant hydrochloride (eg Brinavess): indicated to restore normal heartbeat in patients with recent atrial fibrillation. Indicatively, administer the drug at a dosage of 3 mg / kg by intravenous infusion of 10 minutes. If necessary, proceed with a second administration of the active ingredient (2mg / kg) if the heartbeat has not returned to normal after 15 minutes. Do not exceed 5mg / kg total per day.
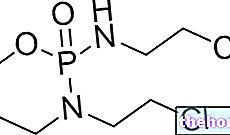
Fluidifiers and anticoagulants:
- Warfarin (eg Coumadin): to be taken for a few weeks, in order to reduce the risk of thrombus and stroke formation. Typically, the administration of this drug follows cardioversion. The dosage must be carefully established by the doctor; in general, it is however recommended to administer the drug maintaining a therapeutic interval between 2 and 3 of INR (prothrombin time). To obtain a higher therapeutic effect, it is recommended to administer the drug in combination with heparin.
- Dabigatran (eg Pradaxa): useful for the prevention of clot formation (therefore thromboembolism) in the context of atrial fibrillation; the efficacy of this drug is comparable to that of warfarin. As we know, blood clots in the arteries can cause stroke, consequently in the context of atrial fibrillation, similar therapy is recommended. Start therapy with a dose of active equal to 110-150 mg, twice daily, orally.
Inhibitor of factor Xa
The drug is used in therapy for its anticoagulant properties, capable of inhibiting one of the factors involved in the mechanism of blood clotting (factor Xa). By blocking factor Xa, thrombin synthesis is denied, which reflexively prevents thrombus formation.
- Rivaroxaban (eg Xarelto): indicated for the prevention of complications from atrial fibrillation, such as venous thromboembolism, especially in patients who have previously undergone knee and hip surgery. The recommended dose is 20 mg, to be taken orally, once a day, with the evening meal.
Digitalis drugs: indicated for heart rate control (in the physiological range 60-100 bpm)
- Digoxin (eg. Lanoxin, Eudigox, Digoss FN): the drug is an antiarrhythmic able to control the heart rate of a patient at rest but NOT during physical activity. Very often patients with severe atrial fibrillation also need calcium- antagonists (eg verapamil, contraindicated, however, in the treatment of atrial fibrillation with pre-excitation and in children), ACE inhibitors or beta blockers, for the treatment of hypertension. For heart rate control in patients with atrial fibrillation, the indicative dose of the drug is 8-12 mcg / kg. The doses of digoxin taken for the treatment of chronic atrial fibrillation must be titrated to the minimum dose, useful to allow the desired therapeutic effect (heartbeat control), without causing severe side effects. The administration of digitalis and antihypertensive drugs reduces the risk of complications of atrial fibrillation.