Definition
Rheumatoid arthritis (RA) is a chronic inflammatory disease, the cause of which seems to go back to an "alteration of the immune system - usually responsible for the body's defense - which activates an abnormal response and develops an inflammatory reaction. This inflammatory process. it involves the joints in an elective way: patients suffering from rheumatoid arthritis complain of joint pain accompanied, especially in the morning, by swelling, stiffness and difficulty in moving. same joint tissues (tendons, muscles) on both sides of the body.
Causes
Rheumatoid arthritis is an autoimmune-based systemic disease, the causes of which are not yet fully known, but various factors that may contribute to its onset have been identified. The pathogenesis is known to be related to an "alteration of the immune system: in genetically predisposed subjects, a triggering event would be responsible for the initiation of the cascade of events that results in joint inflammation. Initially, the target is the synovial membrane that covers the joint. joint and produces the synovial fluid necessary for the lubrication and nourishment of the articular cartilage. Inflammation, therefore, damages the cartilage causing its erosion and, later on, involves ligaments, cartilages, bones and surrounding tissues. deformities that limit the ability to carry out normal daily activities. Rheumatoid arthritis occurs to a greater extent among women, especially those aged between 40 and 60, however, young people can also be affected.
Symptoms
The characteristic symptoms of rheumatoid arthritis are joint pain and swelling, with limited movement and functionality. Stiffness is most intense in the morning, upon awakening, and can last for an hour or more. The joints most commonly affected are those of the fingers and toes, wrists, ankles and knees; more rare is the involvement of the hips, shoulders, elbows and spine. The progressive deformation and damage to the articular structures are followed by extra-articular symptoms, indicative of a systemic involvement of the disease, such as: general fatigue, muscle soreness, loss of appetite, dry eyes and mouth, low fever and general malaise . In addition, small bumps, called rheumatoid nodules, develop under the skin of the elbows, hands and feet. In severe rheumatoid arthritis, visceral nodules may also arise, usually asymptomatic, especially in the lungs.
The information on Arthritis - Rheumatoid Arthritis Drugs is not intended to replace the direct relationship between health professional and patient. Always consult your doctor and / or specialist before taking Arthritis - Rheumatoid Arthritis Drugs .
Medicines
To date, unfortunately, there is no pharmacological treatment universally recognized as effective to definitively treat rheumatoid arthritis; despite this, drugs and some non-pharmacological therapeutic strategies (eg physiotherapy) can control the symptoms, relieve pain and prevent the onset of permanent damage. In the most serious cases, surgery may be the last therapeutic option, in a desperate attempt to correct the joint damage; some patients with severe rheumatoid arthritis require joint replacement.
The key focus of rheumatoid arthritis is not simply symptom control. Therapeutic management of the disease must also and above all take into account the reduction of pathological progression, in order to avoid damage to the joints.
The drugs used in the treatment of rheumatoid arthritis are of different types: non-steroidal anti-inflammatory drugs (NSAIDs) and corticosteroids to control pain and other symptoms; anti-rheumatic drugs modifying the course of the disease (the so-called DMARDs) capable of intervening directly in the pathogenetic mechanisms of rheumatoid arthritis (methotrexate, hydroxychloroquine, sulfasalazine, cyclosporine, azathioprine, etc.) and biological drugs. The ideal treatment of rheumatoid arthritis requires however, a multispecialist approach with the collaboration between rheumatologists, general practitioners, orthopedists, physiatrists and psychologists.
The following are the classes of drugs most used in the therapy against rheumatoid arthritis, and some examples of pharmacological specialties; it is up to the doctor to choose the active ingredient and the dosage most suitable for the patient, based on the severity of the disease, the state health of the patient and his response to treatment:
NSAIDs: first-line therapy uses non-steroidal anti-inflammatory drugs, useful for rapidly reducing joint inflammation and the intensity of symptoms. Although they are capable of relieving pain and controlling the inflammatory process, it should be considered, however, that the long-term administration of NSAIDs can cause more or less serious side effects, such as stomach pain, nephropathies, ulcers, traces of blood in the stool, hypersensitivity reactions. When treating symptoms of rheumatoid arthritis with oral NSAIDs, doctors usually prescribe the lowest effective dose for the shortest possible time; at the same time, he may prescribe a proton pump inhibitor (PPI) and periodically re-evaluate factors that increase the risk of adverse effects. Among the NSAIDs used in the management of rheumatoid arthritis include:
- Acetylsalicylic acid
- Ibuprofen
- Naproxen
- Diclofenac
- Celecoxib
- Etoricoxib
The exact posology required for pain control in the context of rheumatoid arthritis to treat rheumatoid arthritis is prescribed and possibly changed by the physician. The newer COX2 inhibitors (celecoxib, etoricoxib) offer the same beneficial therapeutic effects as NSAIDs, but appear to avoid the risk of ulcers.
Corticosteroids: They reduce inflammation and other symptoms more quickly and to a greater extent than other drugs. However, they cannot prevent joint destruction and their clinical benefits often diminish over time. In addition, long-term administration of corticosteroids systemic to treat the pain associated with rheumatoid arthritis can cause ulcerative gastroduodenal, bruising, weight gain, glaucoma, diabetes mellitus, hypertension and swelling of the face. Do not suddenly stop taking corticosteroids to avoid flare-ups of the disease and long-term side effects, but consult your doctor for advice.
- Prednisone: May slow the rate of joint damage that accompanies rheumatoid arthritis. Prednisone can be administered orally or intra-articularly.
- Dexamethasone: the dose must be established by the doctor after an accurate diagnosis of the patient.
Anti-rheumatic drugs (DMARDs) and immunomodulators: they block the degeneration of the disease by stimulating the immune system. These drugs greatly improve the symptoms, joint function, and quality of life of most patients with rheumatoid arthritis.
- Hydroxychloroquine: antimalarial drug indicated for the treatment of mild rheumatoid arthritis, especially in the initial stages, as well as being widely used in therapy for the treatment of systemic lupus erythematosus. The drug should be discontinued if no improvement is observed after 9 months.
- Chloroquine: chloroquine, like the previous drug, is also used in the treatment of inflammation in the context of moderate rheumatoid arthritis (although used less frequently because it is less tolerated) and in the treatment of lupus erythematosus. For the posology, consult your doctor.
- Methotrexate: drug antagonist of folic acid synthesis, capable of significantly influencing the body's immune response. In this regard, it is widely used in the treatment of rheumatoid arthritis and is well tolerated.
- Sulfasalazine: anti-inflammatory-immunomodulatory drug widely used in therapy for the treatment of rheumatoid arthritis, as it is well tolerated; it can relieve symptoms and slow down the development of joint damage. Sulfasalazine is generally administered in the form of gastro-resistant tablets.
- Azathioprine - the drug belongs to the class of immunomodulators; the maintenance dose should be reduced to avoid side effects and to reduce the risk of toxicity.
Biological drugs: known as biological response modifiers or "biotechnological agents", they act in a selective and specific manner on some molecules produced by cells of the immune system and which cause inflammation and damage to the joints and organs that may be involved. Their use is reserved exclusively for patients with active rheumatoid arthritis, for the failure of conventional therapies, that is, if the use of classic antirheumatic drugs (DMARDs) has not reported any benefit after a few years of treatment. The treatments approved by the most important agencies of the drugs are: infliximab, adalimumab, etanercept, anakinra, abatacept, rituximab, tocilizumab, golimumab and certolizumab. Before starting treatment with biologics, it is important to rule out the presence of underlying or underlying infectious diseases, such as tuberculosis or virus infections. of hepatitis or HIV and neoplasms.
- Adalimumab: tumor necrosis factor alpha (TNF-alpha) inhibitor drug, indicated for the treatment of severe rheumatoid arthritis. For some patients, for greater efficacy, it is recommended to combine methotrexate with this drug.
- Infliximab: drug indicated to treat moderate and severe rheumatoid arthritis; often, the drug is given in combination with methotrexate.
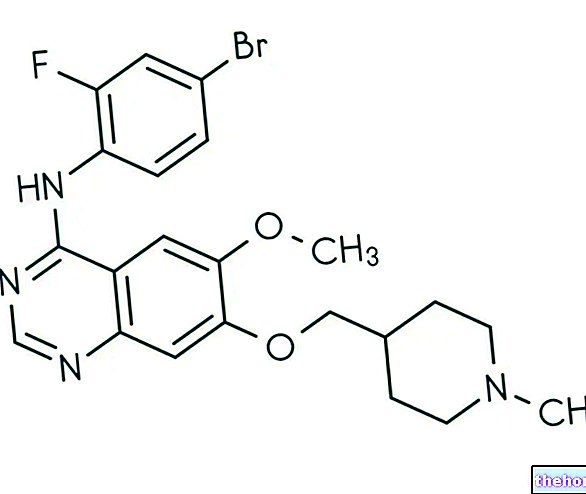
- Tocilizumab or atlizumab: is a humanised monoclonal antibody active against the interleukin-6 receptor (IL-6R), preventing cytokine (IL-6) from exerting its pro-inflammatory effects. Interleukin-6 plays an important role in the immune response and autoimmune diseases, such as rheumatoid arthritis, often see an abnormal increase in its levels. Tocilizumab is able to interact with the soluble form of the IL-6 receptor and the membrane-bound form, acting as an immunosuppressive drug. Sometimes given in combination with methotrexate (if tolerated by the patient), Tocilizumab is used for the treatment of moderate to severe rheumatoid arthritis and systemic juvenile idiopathic arthritis, if other approaches such as disease-modifying antirheumatic drugs (DMARDs) and TNF-alpha inhibitors have been shown to be ineffective or not tolerated. Tocilizumab slows the progression of the disease and can improve the joint function of patients.
Other articles on "Arthritis - Rheumatoid Arthritis Medications"
- Rheumatoid Arthritis: Treatment
- Rheumatoid Arthritis: Diagnosis
- Diet and Rheumatoid Arthritis