Depression and Neurotransmitters
Depression is a serious psychiatric condition that affects many people. It involves the mood, mind and body of patients, who feel hopeless and experience a sense of hopelessness, uselessness and helplessness.

Neurotransmitters are synthesized within the presynaptic nerve termination, stored in vesicles and finally released in the synaptic wall (the space between the presynaptic and postsynaptic nerve terminations) in response to certain stimuli.
Once released from the deposits, the monoamines interact with their own receptors - both presynaptic and postsynaptic - in order to carry out their biological activity.
In this way the transmission of the nerve impulse from one neuron to the other is made possible.
After having carried out their function, the monoamines are picked up by specific transporters and brought back inside the presynaptic nerve termination.
At this point, monoamine oxidase (or MAO) intervenes, which are the enzymes responsible for the metabolism and degradation of monoamines.
Monoamine oxidase inhibitors (or MAOIs) are able to block these enzymes; in this way they increase the concentration - and consequently the activity - of the monoaminergic neurotransmitters. This increase causes the depressive pathology to improve.

History
The discovery of MAOIs occurred by chance, thanks to the development of derivatives of a drug used for the treatment of tuberculosis, isoniazid (hydrazide of nicotinic acid).

Hyproniazid - Chemical Structure
The first analogue of isoniazid to be synthesized was the "iproniazid. During the clinical trial phases of this derivative, a considerable improvement in mood was noted in patients suffering from tuberculosis. However, iproniazid was found to be hepato-toxic at the therapeutic doses necessary to obtain both an "antituberculous action and a" antidepressant.
The discovery of the antidepressant action of iproniazid, however, gave impetus to the search for new inhibitors of monoamine oxidase. This impulse led to the synthesis of hydrazine derivatives and non-hydrazine derivatives with lower toxicity than iproniazid.
Classification
The classification of monoamine oxidase inhibitors can be done basically in two ways.
The first subdivision is the one that divides MAOIs into:
- Hydrazine derivatives, such as phenelzine;
- Non-hydrazine derivatives, such as tranicylpromin, chlorgiline and selegiline.
The second classification is that carried out on the basis of selectivity or not towards the various isoforms of monoamine oxidase.
In fact, two isoforms of MAO are known, the monoamine oxidase type A (MAO-A) and those of type B (MAO-B).
MAO-A and MAO-B differ in their specificity towards certain substrates and in the different distribution within the tissues of the organism. Based on this subdivision we can therefore distinguish:
- Non-selective and irreversible inhibitors of MAOs, such as phenelzine and tranicylpromin;
- Selective MAO-A inhibitors, such as moclobemide;
- Selective MAO-B inhibitors, such as selegiline. However, this drug is not so much used in the treatment of depression, but in the treatment of Parkinson's disease which is characterized by a reduced central dopaminergic transmission in the nigrostriatal areas.
Mechanism of action
Monoamine oxidases are enzymes mainly found in nerve tissues, liver and lungs.
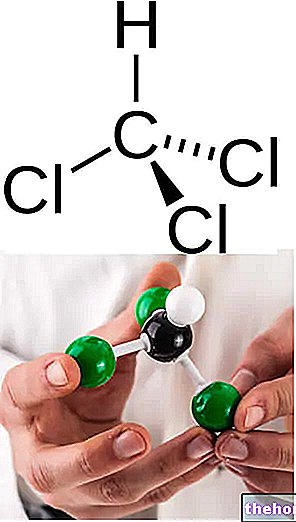
Their task is to catalyze the oxidative deamination (ie the elimination of amino groups) of some endogenous substrates (monoamines), including adrenaline, noradrenaline, serotonin, dopamine, tyramine and phenylethylamine.
As mentioned, two isoforms of monoamine oxidase are known, the MAO-A and the MAO-B which differ in their specificity towards particular monoamines and in their distribution in different tissues.
- MAO-A's are more selective for the metabolism of norepinephrine and serotonin.
- MAO-B, on the other hand, show greater selectivity for the metabolism of tyramine and dopamine.
The other monoamines are metabolized by both isoforms without particular selectivity.
Regardless of the type of enzymatic isoform that is inhibited, the mechanism of action of MAOIs is always the same. These drugs are able to inhibit monoamine oxidase preventing metabolism and degradation of endogenous monoamines.
If the monoamines are not metabolized, their concentration increases; therefore, their biological activity also increases. This leads to an improvement in the depressive pathology.
However, before carrying out their pharmacological action, MAOIs may need a first latency period ranging from a few days to a few months.
On the other hand, once triggered, the antidepressant effect can last even weeks after the interruption of therapy.