What is Hypercapnia?
Hypercapnia is the medical term used to refer to an excess of carbon dioxide in body fluids, particularly the blood.
Often, but not always, this condition goes hand in hand with hypoxia, that is the lack of oxygen in the whole organism or in one of its areas, and with hypoxemia (lack of oxygen available in the blood).
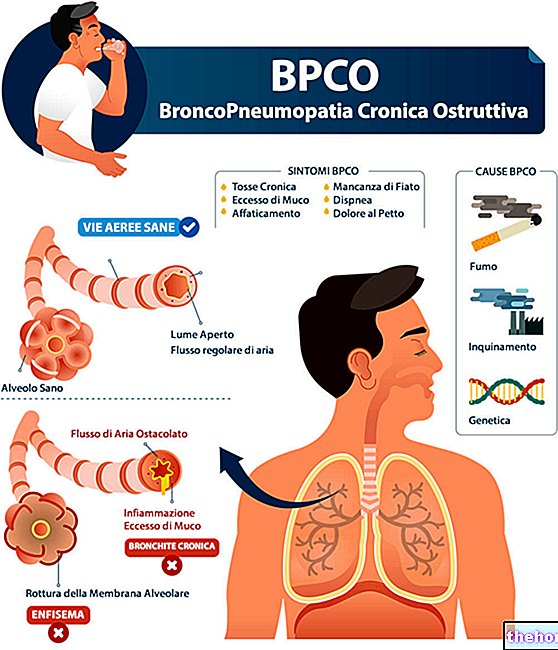
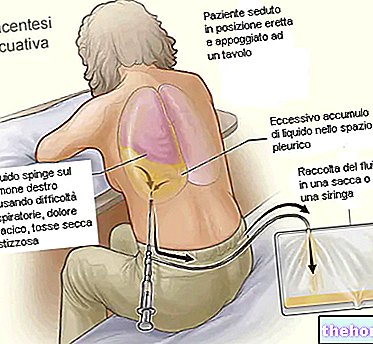
Causes
Hypercapnia is generally caused by hypoventilation, pulmonary diseases, cardiocirculatory insufficiency (inability of the heart to supply blood to the various parts of the body in sufficient quantities) and living in environments particularly rich in carbon dioxide.
Carbon dioxide in the blood
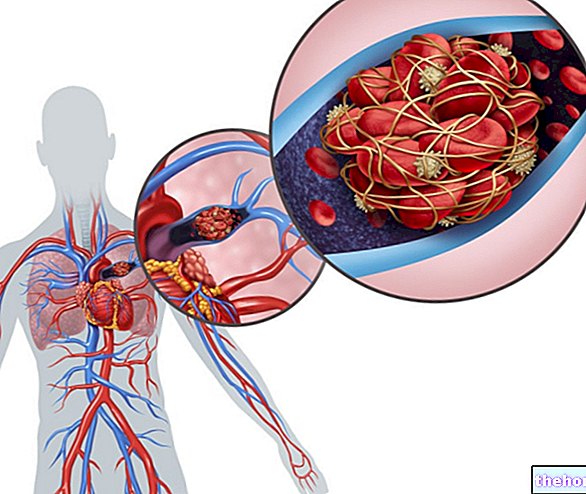
About 7% of the carbon dioxide present in the circulation is dissolved in venous blood; the remaining 93% diffuses into red blood cells; here 70% is converted into bicarbonate ion and the remaining 23% binds to hemoglobin.
CO2 is a waste product and its excess in the circulation lowers the pH of the blood significantly, causing a disorder known as acidosis. Extremely high levels of CO2 in the blood interfere with the hydrogen bonds of molecules and can denature proteins.
At the pomonary level, the carbon dioxide is removed from the blood, since the PCO2 of the atmospheric air is much lower than the venous one, so that there is a passage of the gas from the point of greatest concentration (venous blood) to the poorest compartment. CO2 (the ambient air present in the pulmonary alveoli).
Normal Values
Under normal conditions, the blood concentration of carbon dioxide - expressed as partial pressure of CO2 - is approximately equal to 45 mmHg (in venous blood). Beyond this level we speak of hypercapnia.
Consequences of Hypercapnia
When the concentration of carbon dioxide increases beyond the normal threshold, the subject goes into hyperventilation, then breathes more deeply and frequently, experiencing the so-called dyspnea or hunger for air.
These symptoms become particularly evident, and led to exasperation, when the PCO2 reaches levels close to 60-75 mmHg; once this threshold is exceeded, in addition to ventilating as often and deeply as possible, the subject affected by hypercapnia becomes lethargic, confused and in some cases semicomatous.
Anesthesia and death occur when the PCO2 reaches values between 120 and 150 mmmHg.
In similar conditions, carbon dioxide exerts a depressive action on respiration, thus activating a vicious circle that feeds the accumulation of carbon dioxide, leading to further respiratory depression, therefore to an increased accumulation of carbon dioxide, and so on. This cycle is repeated until it rapidly culminates in the death of the subject due to respiratory failure.


.jpg)