Causes
Atrophic vaginitis is caused by a reduction in estrogen levels, in turn a consequence of: menopause, breastfeeding, chemotherapy drugs, radiotherapy, drugs for the treatment of endometriosis and uterine fibroids, therapy for breast cancer.
Symptoms
In atrophic vaginitis the vaginal mucosa becomes thin, fragile and more exposed to the risk of infections. The characteristic symptoms of atrophic vaginitis are: vaginal burning / dryness, dyspareunia, urinary incontinence, leukorrhea, bleeding after intercourse, vaginal itching.
Diagnosis
The hypothesis of atrophic vaginitis is ascertained by pelvic examination, pap smear, vaginal swab and urinalysis.
Therapy
Symptoms of atrophic vaginitis can be alleviated by following specific estrogen therapy. Usually, the doctor also recommends the application of lubricating creams as a remedy for vaginal dryness and itching.
of estrogen.
Not surprisingly, atrophic vaginitis is also known as climacteric vaginitis: during menopause, in fact, the woman undergoes an "inevitable alteration of the hormonal structure, in which the levels of estrogen - and especially progesterone - are extremely low, while the dosage of FSH (follicle stimulating hormone) and LH (luteinizing hormone) shows high values.
The above does not exclude that atrophic vaginitis can also occur outside the menopausal period. In fact, some women complain of the same discomfort in the post-partum period, during breastfeeding or following the surgical removal of the ovaries.
- they guarantee physiological vaginal lubrication, thus keeping the genital mucosa healthy and in good condition. Precisely because of the estrogen reduction, in atrophic vaginitis the vaginal mucosa thins, becomes less elastic, more fragile, less lubricated and more susceptible to inflammation.
In most cases, atrophic vaginitis occurs in the case of physiological changes such as:
- Menopause, the main cause of atrophic vaginitis;
- Breastfeeding;
- Early menopause (the characteristic symptoms of menopause appear before the age of 40).
In some women, however, the reduction in estrogen does not depend on physiological changes in the body; rather it is a consequence of surgery, drug therapies or serious pathologies:
- Medicines for the treatment of endometriosis and uterine fibroids. In these cases, atrophic vaginitis arises as a side effect of specific drug therapy.
- Some women have to undergo surgical removal of the ovaries or uterus (hysterectomy): inevitably, similar interventions block the synthesis of estrogen, thus causing atrophic vaginitis.
- Alterations of the immune system.
- Breast Cancer Medications.
- Impaired function of the ovaries due to chemotherapy / radiotherapy.
Finally, remember that there are cases in which atrophic vaginitis is idiopathic; in other words, it is not possible to trace any precise cause.
What are the Risk Factors for the Development of Atrophic Vaginitis?
Some predisposing factors for atrophic vaginitis have been identified.
First of all, the habit of smoking: smoking damages the correct circulation of the blood, partly depriving the tissues (including the vaginal one) of the oxygen necessary for proper metabolism. It should not be forgotten that smoking interferes with the normal synthesis of estrogen.
Furthermore, it has been observed that women who smoke tend to enter menopause earlier than women who do not smoke, therefore they are more prone to early atrophic vaginitis.
A scientific study noted an "interesting" coincidence: mothers who gave birth to their children by caesarean section are more prone to vaginal atrophy than those who gave birth naturally (vaginally).
;Furthermore, the presence of atrophic vaginitis increases the risk of bacterial and fungal infections of the genitals.
Furthermore, the psychological impact induced by physical symptoms should not be forgotten. Some women in menopause who undergo atrophic vaginitis, in fact, finding themselves in a period that is already delicate in itself, could become anxious, irritated and stressed.
In some cases, however, vaginal atrophy occurs so slowly that women do not experience any symptoms until 5-10 years after the onset of menopause.
, in order to trace the triggering cause and possibly choose whether to intervene pharmacologically or not.
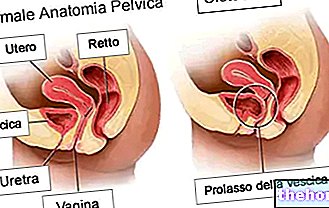
The pelvic examination is particularly indicated for this purpose: the gynecologist examines the internal and external genitals of the woman, checking for any signs of vaginal dryness, redness and / or local irritation and evaluating a possible prolapse of the pelvic organs.
The Pap test - which involves the collection of a sample of cervical cells for a subsequent laboratory cytological examination - diagnoses the presence of a possible tumor in the cervix.
The vaginal swab is also an important investigative test, used in case of suspected atrophic vaginitis: it identifies any pathogens in the vaginal and cervical flora, and detects the pH of the vaginal microenvironment. We remember, in fact, that in atrophic vaginitis the vaginal pH is generally altered (higher than normal, therefore less acidic).
The urine test is indicated when the woman complains of urinary symptoms.
The most commonly used is estradiol which can also be associated with norethisterone, drospirenone, cyproterone, levonorgestrel or medroxyprogesterone.Medicines based on the aforementioned active ingredients can be formulated as:
- Transdermal gels;
- Trandermal patches;
- Skin sprays;
- Tablets to be taken by mouth;
- Vaginal tablets.
To alleviate the disorder, it is possible to apply specific lubricating creams on the vaginal mucosa: these products, while not acting on the triggering cause, are an effective remedy to relieve vaginal dryness induced by atrophic vaginitis.
In some women, atrophic vaginitis is accompanied by urinary symptoms such as incontinence: in such circumstances, regular Kegel exercises may be useful to strengthen the pelvic floor and bladder muscles. Kegel exercise is also indicated. as a remedy for pelvic organ prolapse: many postmenopausal women also complain of this disorder associated with atrophic vaginitis.