The Virchow triad owes its name to the German physician Rudolph Virchow who, in 1856, clarified the etiology of pulmonary embolism in one of his publications.
Did you know that ...
Although Virchow contributed to describing the pathophysiology related to pulmonary embolism, it was not he who proposed the drafting of the aforementioned triad. However, for unclear reasons, several years after the death of the German doctor (approximately, around the 1950s), the triad was developed and named after him. On the other hand, it is also true that Virchow, in the drafting of his work, referred to the various factors that can contribute to the formation of thrombi; however, those same factors were not highlighted for the first time by the German doctor, but by other doctors before him.
:
- Endothelial damage;
- Abnormalities or alterations in blood flow (stasis and turbulence);
- Hypercoagulability.
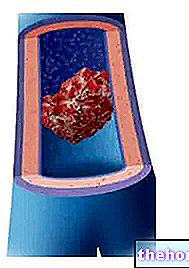
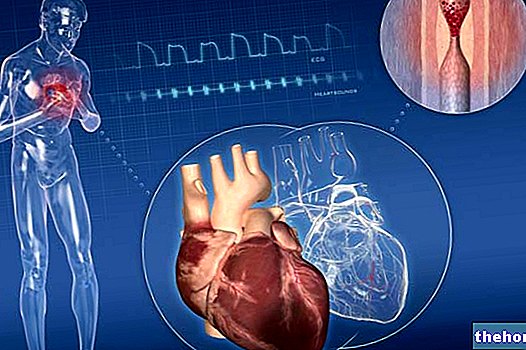
The Virchow triad, therefore, represents a tool that can prove to be very useful for doctors in understanding what are the causes and factors that contribute to the formation of thrombus, therefore, that contribute to the development of both venous and arterial thrombosis.
Below, the aforementioned factors will be analyzed in more detail.
and arteries.The endothelium is the inner lining of the blood vessels, the heart and the lymphatic vessels. It is made up of the so-called endothelial cells and performs numerous functions, including:
- Barrier function;
- Regulation of coagulation, platelet aggregation and fibrinolysis;
- Regulation of inflammatory processes;
- Control and modulation of vascular tone and permeability.
The functions of the endothelium are therefore multiple, all essential for the correct functioning of the cardiovascular system and beyond. It should be noted the role played by the tissue in question in the regulation of coagulation, thanks to which it is possible to prevent the formation of thrombus (antithrombotic action). In the event that damage to the endothelium should occur, however, the so-called endothelial dysfunction would occur which would lead to a decrease in antithrombotic activity in favor of an increase in pro-thrombotic and pro-inflammatory activity, with consequent thrombus formation.
The causes that can lead to the appearance of the endothelial damage mentioned in the Virchow triad can be many, among these we remember:
- Physical injury of the endothelium;
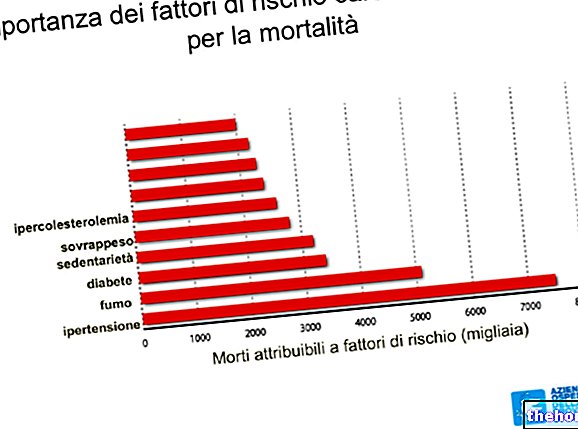
- Hypertension;
- Turbulence of blood flow;
- Inflammatory agents;
- Radiation exposure;
- Metabolic abnormalities, such as homocysteinemia and hypercholesterolemia;
- Absorption of toxins from cigarette smoke.
Please Note
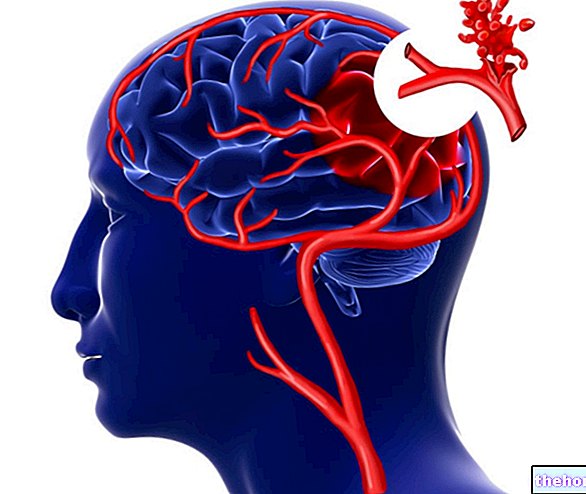
While according to some authors the alterations in the endothelium play a marginal role in the onset of thrombi compared to the other two factors of the Virchow triad; according to others, it plays a fundamental role, in particular at the cardiac and arteriolar level. In fact, in the absence of endothelial damage, the high speed of blood flow in the heart and arteries could prevent platelet adhesion and could dilute the clotting factors, thus preventing thrombus formation. Not surprisingly, as mentioned, endothelial damage is one of the determining factors in the formation of thrombus in the arteries and in the heart.
which, therefore, is in contact with the endothelium and tends to flow more slowly.In the presence of anomalies in the blood flow, however, this no longer flows in an orderly manner, but assumes a chaotic motion and / or undergoes a strong slowdown. More precisely, the turbulence of the blood flow is able to cause endothelial damage and dysfunction and is capable of giving rise to countercurrents and local pockets in which the stasis of the same blood occurs.
The presence of the aforementioned anomalies is the cause of an "altered gene expression at the level of the endothelial cells which are found to produce greater quantities of pro-coagulating factors.
Furthermore, when stasis is present, the platelets come into contact more easily with the endothelium, the activated coagulation factors accumulate and the influx of anticoagulant factors is reduced with consequent thrombus formation. Among the possible conditions that can give rise to the stasis of the blood flow, we remember:
- Aneurysms;
- Acute myocardial infarction;
- Mitral valve stenosis and atrial fibrillation;
- Polycythemia;
- Sickle cell anemia.
To be more precise, the term "hypercoagulability" is used to indicate any type of alteration, anomaly or defect in the coagulation pathways that predisposes patients suffering from it to thrombus formation.
In this regard, we remind you that it is possible to distinguish two different types of hypercoagulability, that is, a genetic hypercoagulability and an acquired type.
Genetic hypercoagulability is generally caused by the presence of point mutations located on the genes encoding coagulation factor V and prothrombin.
Acquired hypercoagulability, on the other hand, can occur due to various factors, including:
- Increase in estrogen levels (for example, during pregnancy or by taking oral contraceptives): the increase in this type of hormones, in fact, could induce an increase in the hepatic synthesis of coagulation factors by reducing the synthesis of antithrombin III;
- Presence of some malignant tumors;
- Presence of stasis and vascular lesions;
- Cigarette smoke;
- Obesity;
- Heparin-induced thrombocytopenia syndrome: this is a particular syndrome that develops in some patients on anticoagulant therapy based on unfractionated heparin and which leads to the onset of a pro-thrombotic state.
- Antiphospholipid antibody syndrome.