Key points
Behçet's disease (or syndrome) is a rare and complex multi-system disorder involving small and large blood vessels. It is a chronic / relapsing vasculitis with multiorgan involvement, potentially fatal.

Behçet's disease: causes
Unproven hypothesis: Behçet's disease derives from an "abnormal autoimmune response, triggered in turn by an infectious agent (not yet identified). Risk factors: environmental and genetic factors, cigarette smoking
Behçet's disease: symptoms
Mouth ulcers and ulcers; cataracts, glaucoma and uveitis; genital sores / scars; papulo-pustular lesions of the skin; aneurysm, arrhythmias, leg and arm edema and deep vein thrombosis; Diarrhea, dysphagia, flatulence and gastric ulcers; Inflammation of the brain and nervous system; Arthritis and arthralgia
Behçet's disease: drugs
The treatment currently available is aimed at the mere control of symptoms: cortisone drugs, colchicine, tumor necrosis factor antagonists, NSAIDs.
Behçet's disease
Behçet's disease is a rare complex multisystem syndrome, of unknown etiology, characterized by an "inflammation involving the blood vessels of every anatomical site. Although it is not fully demonstrated, it seems that Behçet's disease has an" autoimmune origin. However, it seems that an intertwining of environmental and genetic factors heavily affects the onset of the disease.
Involving the entire reticulum of blood vessels, the characteristic symptoms of Behçet's disease can be multiple and heterogeneous: oral ulcers, eye inflammation, CNS disorders, skin rashes, genital sores and joint pain. In any case, the symptom picture derived from Behçet's disease varies from person to person.
The specific treatment of Behçet's disease essentially aims at the prevention of serious complications, including blindness.
Behçet's disease bears the name of the discoverer. In 1937 the Turkish dermatologist H. Bechet observed the recurrence of a symptomatological triad in many patients: oral ulcers, frequent genital sores, and ocular inflammation (uveitis) were considered three characteristic features of the same disease.
Incidence
Behçet's disease is more common in patients aged between 15 and 45 years; in particular, in subjects under the age of 25 the target of the disease seems to be the eye. Despite what has been said, Behçet's syndrome can also begin during the pediatric age and in senescence.
From recent statistics reported in the Scientific journal Expert opinion on pharmacotherapy, it is clear that Behçet's disease manifests itself with a prevalence of 0.3-6.6 cases per 100,000 healthy inhabitants, with a marked prevalence in China, Japan and the Middle East in general. Males appear to be more affected than women.
Causes
As mentioned in the incipit, a precise cause implicated in Behçet's disease has not yet been identified. The syndrome is not contagious, let alone infectious and cannot be transmitted by sexual contact. However, it seems that the etiopathogenesis of the syndrome derives from a "abnormal autoimmune response: the body, by mistakenly recognizing some (healthy) cells as" foreign and potentially dangerous ", triggers an exaggerated defensive reaction against them, causing damage. It is thought possible that an infectious agent - or another unknown element - could trigger this exaggerated autoimmune inflammatory response, the main target of which is the vessel wall.
It should not be forgotten that some environmental and genetic factors can predispose the patient to Behçet's disease: the hypothesis according to which there is a genetic correspondence with the HLA-B51 antigen and with the HLA-B57 seems to be supported.
Among the predisposing factors of Behçet's Syndrome we remember the cigarette smoke: the chemical substances contained in it can in some way damage the DNA, therefore predispose the patient to the disease.
General symptoms
Being a systemic disease, Behçet's syndrome can also spread to all visceral organs - lung, stomach, intestine, etc. - up to involve muscles and nerves.
The distinctive symptoms of Behçet's disease vary from person to person. Furthermore, even the frequency of appearance of the signs is purely subjective: some patients constantly complain of the presence of the disease, while in others the symptoms reappear less frequently.
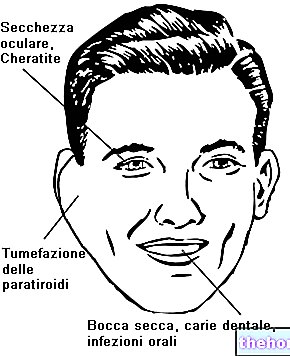
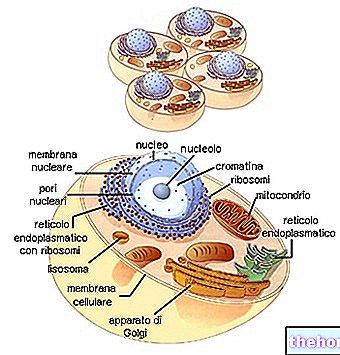
The location of the disease considerably affects the intensity of the symptoms: the most involved anatomical sites are the mouth, eyes, genitals, skin, vascular system, digestive system, brain and joints.
Symptoms table
Although less frequently than the symptoms listed above, patients with Behçet's syndrome experience seizures.
Behçet's disease can give a poor prognosis: in fact, the possible rupture of vascular aneurysms and heavy neuronal lesions can seriously endanger the patient's life.
Diagnosis
The diagnostic assessment of Behçet's disease is rather complex, considering the heterogeneity of the symptoms and the affinity with many other pathologies.
The peculiarities of this disease - mouth ulcers and genital ulcers - may suggest this condition. The detection of inflammation of the pulmonary arteries can also be a strong indicator of Behçet's syndrome.
Particular is the "diagnostic analysis called" patergic test "(Pathergy test): the doctor proceeds by intradermally injecting a physiological solution or simply pricking the patient's skin with a sterile needle. If after 48 hours a lump forms in that exact spot, Behçet's syndrome is conceivable. The mechanical stimulus exerted by the needle favors the formation of a pustular lesion: in such circumstances, the patient will be considered positive for Behçet's disease. A further biopsy can support the diagnosis.
No diagnostic test can definitively and with absolute certainty ascertain or deny Behçet's disease. The hypothesis can be demonstrated through the symptomatological investigation and the verification of some tests.
Therapy
Unfortunately, since it is a rare disease, the large pharmaceutical companies do not seem to consider Behçet's syndrome a target of interest for investing in research.
However, the treatment currently available is aimed at controlling symptoms IF AND WHEN they appear. The drugs used in therapy are purely anti-inflammatory. Colchicine, cortisones, immunosuppressants and NSAIDs seem to excellently attenuate symptoms:
- Cortisones: applied directly to damaged skin (oral ulcers, genital lesions, eye diseases, etc.) reduce inflammation. They are probably the most widely used drugs in therapy for Behçet's disease. However, there is no proven evidence on the effectiveness of these. drugs in reducing the progression of the disease.
- Colchicine (eg. COLCHICINE LIRCA): drug used for the treatment of gout. In Behçet's disease, the drug is useful for reducing joint pain.
- Immunosuppressants (eg azathioprine, chlorambucil or cyclophosphamide): they exert their therapeutic activity by suppressing the immune system (hyperactive), thus reducing inflammation.
- Tumor necrosis factor antagonists (eg etanercept or infliximab): currently little used, the use of these drugs should be evaluated in patients with Behçet's disease with severe skin, genital / oral (ulcers and papules) and ocular involvement .
- NSAIDs: temporarily reduce pain and inflammation
The administration of anticoagulants or antiplatelet agents does not seem to have any positive outcome in the prevention of vascular complications (eg deep vein thrombosis) in the context of Behçet's disease.