What is Propionibacterium acnes
Propionibacterium acnes is a Gram-positive anaerobic, non-spore-forming bacterium that normally resides in human skin, in particular in the pilosebaceous follicles, where it draws the nutrients it needs from sebum, from the by-products of skin metabolism and from the cellular debris present in these areas.

Role in Acne
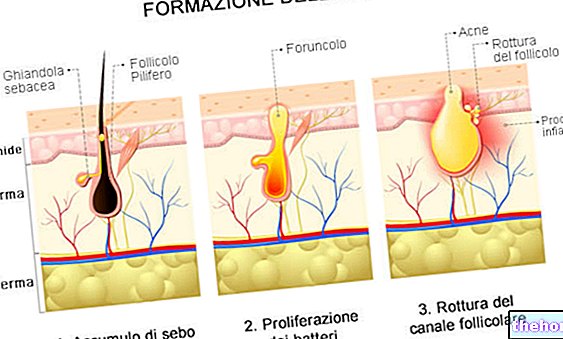
Propionibacterium acnes prefers conditions of anaerobiosis (absence of oxygen) associated with the presence of abundant sebaceous secretions; these circumstances materialize inside the comedones ("plugs of the skin pores"), miniature black points that prevent the normal flow of sebum into the duct of the pilo-sebaceous follicle, and from there to the skin surface.
The activity of the Propionibacterium acnes inside the comedones it determines an inflammatory response mediated by the release of various substances capable of playing a role in the pathogenesis of acne: hyaluronidase, protease, lipase and chemotactic factors for neutrophils, lymphocytes and macrophages. Well known, in this regard, is the ability of the Propionibacterium acnes to produce an extracellular lipase that hydrolyzes the triglycerides of the sebum to glycerol and fatty acids, favoring the growth of other bacterial species, predisposing to comedogenesis and aggravating local inflammation. This inflammation undermines the integrity of the keratinocytes and the follicular wall, damaging it up to to cause it to break.
In some subjects, the skin inflammatory reaction to these events is such as to trigger an exponentially growing inflammatory reaction, which culminates in the typical signs of acne: formation of papules, pustules and nodules.
Treatment
For the important role of the Propionibacterium acnes in the etiopathogenesis of acne, antibiotics - both topical and systemic - constitute an important aid in the pharmacological therapy of acne, especially the pustular one.
Normally, the use of topical antibiotic therapy is reserved only for the most severe cases of acne, even more so in the case of oral antibiotic therapy, in order to avoid the establishment of resistance to the same antibiotics.
In fact, although the bacteriostatic, bactericidal and anti-inflammatory action of these drugs is therapeutically advantageous, the growth of strains of Propionibacterium acnes resistant to some of the antimicrobials normally used in topical therapy, such as clindamycin, erythromycin, benzoyl peroxide, meclocycline, nadifloxacin, gentamicin and azelaic acid.
For this reason, the use of antibiotics must be in full compliance with medical prescriptions. Generally, the treatment of acne with topical antibiotics should be limited to a period of 6-8 weeks and, above all, these drugs should not be used. in monotherapy.
Topical retinoids (such as adapalene, tretinoin or isotretinoin) increase the anti-acne efficacy of antimicrobials by facilitating their penetration into blocked pilosebaceous follicles, where the Propionibacterium acnes.
Other pathologies
The Propionibacterium acnes it is not implicated solely and exclusively in the onset or worsening of acne manifestations.
In fact, this beating can also become an opportunistic pathogen, occasionally identified as responsible for arthritis, osteomyelitis, endocarditis, meningitis and surgical infections (being protected inside the pilosebaceous follicles, it resists very well to preoperative skin disinfection procedures).
Furthermore, some studies have highlighted the presence of P. acnes in patients with sarcoidosis and sciatica, thus hypothesizing a relationship between these pathologies and the presence of a possible infection caused by this beating.
In patients with sarcoidosis, the P. acnes it was found inside the lymph nodes. In patients suffering from sciatica, however, the beating was found in the intervertebral discs.
Finally, the inflammation caused in the skin by the Propionibacterium acnes can create favorable conditions for the development of secondary infections by other bacteria that are not normally part of the skin commensal flora, such as, for example, the Staphylococcus epidermidis.




























