Ulcerative Colitis
Ulcerative colitis, also called ulcerative colitis, is a chronic inflammatory disease affecting the mucosa of the large intestine (colorectal).

NB. It is also quite common to find strong emotional stress probably caused by the anxiety-inducing tendency of some subjects suffering from ulcerative colitis. This etiology seems to be comparable to that of irritable bowel syndrome.
Ulcerative colitis manifests itself with MUCOEMATIC diarrhea, that is, containing a good amount of intestinal mucus associated with blood; diarrheal discharges are more frequent at night and after meals, and are associated with CRAMPIFORMING ABDOMINAL PAIN and a feeling of constant need to defecate even though the rectum is already completely empty (TENESMUS).
If left untreated, ulcerative colitis can cause the affected mucosal area to expand. with relative worsening of symptoms. In addition to enteric manifestations, high fever is common.
Treatment of ulcerative colitis focuses primarily on inducing remission, and on maintaining and managing any complications related to the disease.
The role of diet in ulcerative colitis
The most important trick in the prevention of ulcerative colitis is undoubtedly to maintain INTEGRAL the intestinal mucosa; however, the diet for ulcerative colitis changes significantly according to the state of the disease, or better:
if the ulcerative colitis is found in latent form, when it does NOT present the specific symptoms, the goal of the diet is to MAINTAIN the intestinal balance BY AVOIDING acute symptoms; on the contrary, if ulcerative colitis manifests acute symptoms, the goal of the diet is to reduce enteric manifestations.
Diet in the stages of remission
In the period of latency or remission, the dietary therapy of ulcerative colitis aims at maintaining intestinal efficiency and at strengthening the "barrier effect" towards pathogens, acidity, food waste, etc.
Colon peristalsis is favored by the right amount of dietary fiber, which should be introduced in the right doses and as regularly as possible. In this regard, the research institutions recommend taking about 30g / day (+/- 5g), a portion which, based on subjectivity, can be increased or decreased based on the peristaltic response individual (frequency of evacuation and consistency of faeces). The fiber, adequately divided between soluble (mostly contained in fruit and vegetables) and insoluble (mainly from cereals and derivatives), in addition to maintaining a certain "vitality" of the colic muscles, nourishes the physiological bacterial flora, significantly contributing to the maintenance of the right trophism bacterial. Since these are molecules also useful for the growth of physiological colonies (function PREbiotic), foods containing fiber act synergistically to PRObiotics (yogurt, fermented milks, supplements, drugs, etc.) for the maintenance of the mucosal defenses; in the event that the patient does not use probiotic foods, consulting the doctor it is possible to integrate the contribution of these bacterial strains with drugs or food supplements containing: L. acidophilus, B. bifidum, L. bulgaricus.
Dietary sources of omega-three (for the powerful anti-inflammatory action of these essential fatty acids), and those of glutamine, for the trophic function of this amino acid on the intestinal mucosa, are also particularly recommended in the diet of subjects suffering from ulcerative colitis.
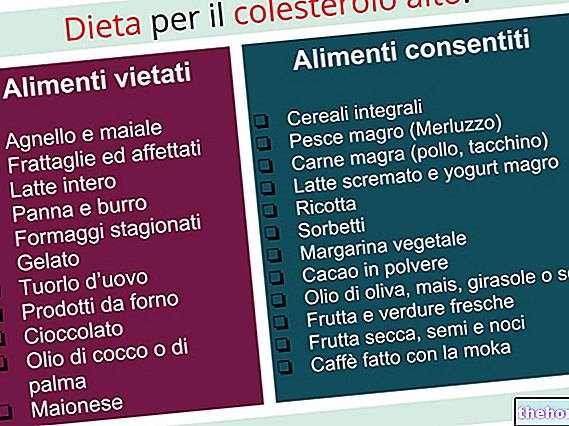
Finally, remember that all IRRITANT agents for the mucosa must be limited in the diet, therefore, if possible, it is advisable to drastically REDUCE alcohol, coffee, strongly spiced foods, very fatty foods, etc.
Diet in the acute stages
On the other hand, in the period of acute ulcerative colitis dietary recommendations change drastically. Having to comply with the increased water requirement (dehydration induced by diarrhea), the first precaution is to introduce WATER frequently; moreover, remember that mucoematic diarrhea favors nutritional malabsorption, therefore, it may be necessary to supplement vitamins associated with mineral salts (especially magnesium and potassium). Furthermore, in order to reduce diarrheal discharges as much as possible, in acute ulcerative colitis it is necessary:
- Reduce as much as possible the intake of dietary fiber which, although necessary during maintenance, in the acute phase could favor evacuation, worsening the symptoms.
- Discontinue any PRObiotic integration for HYGIENIC reasons; we know that probiotic bacteria are NOT potential pathogens, however, considering that traces of blood are present in the faeces to indicate a lesion of the walls, for safety it is advisable not to favor the introduction of other bacteria with power.
- Eliminate LACTOSE from the diet as, due to the flaking of the mucosa, it is possible that lactose fermentation is favored by intestinal bacteria; all this would inexorably worsen the frequency and importance of the diarrhea typical of ulcerative colitis.
- Obviously, more than in the latent phase, it is important to ELIMINATE all foods that bring irritating molecules: alcohol, coffee, other nerves, irritating spices (especially pepper), food cooked on the grill or worse on embers, excessively fatty foods, sources of solanine, etc. .
NB: in the most severe cases it may be necessary to replace the diet with parenteral nutrition; at the end of the most intense period, the ulcerative colitis patient will have to reintegrate food a little at a time through an elementary diet (hypoallergenic foods and simple cooking) possibly with low residual slag.
Bibliography:
- Systemic internal medicine - C. Rugarli - Elsevier Massono - page 701















.jpg)











