Hyperthyroidism occurs when there is an excessive production of thyroid hormones. In other words, the thyroid works too much and becomes overactive.
The excess of thyroid hormones released in the blood causes an increased exposure of the target organs to their action. This determines, among other things, a surge in the metabolic processes regulated by these hormones. The heartbeat accelerates, body fat and muscles are reduced, the subject tends to sweat and suffer from hot environments. The nerves tense, the pace becomes frenetic, anxiety comes into play, even paranoia.
Various pathological conditions result in an overproduction of hormones by the thyroid gland. A first distinction that we can make on the origin of hyperthyroidism is between the primary form and the secondary form. Primary hyperthyroidism depends on a thyroid disorder, while the secondary form is caused by a pathology in the pituitary gland, for example a pituitary adenoma that overproduces thyroid stimulating hormone or TSH. I remind you that the TSH produced by the pituitary gland regulates the activity of the thyroid gland and, if produced in excess, overstimulates the gland, which, in response, secretes more thyroid hormones.
As we have anticipated, hyperthyroidism can have different causes.
The most common is called Graves' disease or toxic diffuse goiter. Graves' disease is an autoimmune disease; in practice, the immune system produces abnormal antibodies, which act like TSH by stimulating the thyroid to produce and secrete more hormones. This stimulus can cause a swelling of the neck, the so-called goiter, which is due to the enlargement of the thyroid gland due to an excess of TSH.
Other relevant causes of hyperthyroidism are toxic multinodular goiter and toxic uninodular goiter (or Plummer's disease). In these cases, one or more limited areas of the thyroid become hyperfunctional, therefore able to secrete greater quantities of T3 and T4 (which are the abbreviations with which the two thyroid hormones are identified: thyroxine is T4, while triiodothyronine is the T4).
More rare are the forms of hyperthyroidism associated with thyroiditis, which are inflammatory processes affecting the thyroid. Due to this inflammation, the follicular cells of the gland are injured by pouring an excess of thyroid hormones into the circulation.
Sometimes hyperthyroidism is caused by certain medications, such as an excessive intake of thyroid hormones for weight loss or incorrect treatment of hypothyroidism. Finally, there are cases in which hyperthyroidism is the consequence of some cancers thyroid or pituitary glands or iodine abuse after a period of mineral deficiency.
The symptoms that characterize hyperthyroidism are due to the excessive presence of thyroid hormones in the blood. The greatest expressions are recorded on the neurological, cardiac and, obviously, on the metabolic level. Often, the first physical sign that can be noticed is the enlargement of the thyroid gland, which we have seen to be goiter. This swelling can result in difficulty swallowing and the sensation of having a "bite stuck in the throat".
The presence of constant and excessive thyroid function can also cause weight loss, muscle weakness, insomnia, tremors, hair loss, intestinal hypermobility up to diarrhea, increased sweating and poor tolerance to heat.
People with hyperthyroidism have limited energy reserves and tire easily. The effects on the nervous system make the individual nervous, restless, hyper-excitable and subject to a heightened emotionality. In the heart, on the other hand, high levels of thyroid hormones can cause serious dysfunctions, such as palpitations, tachycardia, increased blood pressure and heart rate, atrial fibrillation and heart failure. The eyes may appear enlarged and bulging, so much so as to give the face an "apprehensive or alarmed" expression.
The protrusion of the eyeballs, which doctors call exophthalmos, is often associated with ocular disorders, such as conjunctival irritation and photophobia (which is intolerance to light). In women there is an alteration in the rhythm of the menstrual cycle; in men, on the other hand, there is a reduction in libido and gynecomastia, which consists of an increase in the volume of the breasts.
When the doctor suspects that there is some thyroid problem, he first examines the anterior region of the neck to look for signs of a diffuse or circumscribed increase in volume as occurs in the presence of a lump, which can appear as a more or less noticeable small lump. on palpation. Secondly, the doctor orders tests to measure thyroid function. A simple blood test makes it possible to measure thyroid hormones and the pituitary hormone that regulates their concentration, the so-called TSH.
Higher than normal levels of thyroxine and triiodothyronine suggest a diagnosis of hyperthyroidism.
Even lower than normal TSH values indicate excessive thyroid activity or a malfunction of the pituitary gland. Little TSH, in fact, means that the pituitary is trying to put the reins on an overactive thyroid.
Furthermore, in the event of suspicion of hyperthyroidism, the determination of thyroglobulin values is useful. It is a protein produced by thyroid cells that participates in the synthesis of thyroid hormones and which in the case of hyperthyroidism is often elevated.
The dosage of antibodies against the thyroid allows, however, to confirm or exclude the presence of autoimmune thyroid diseases such as Graves' disease.
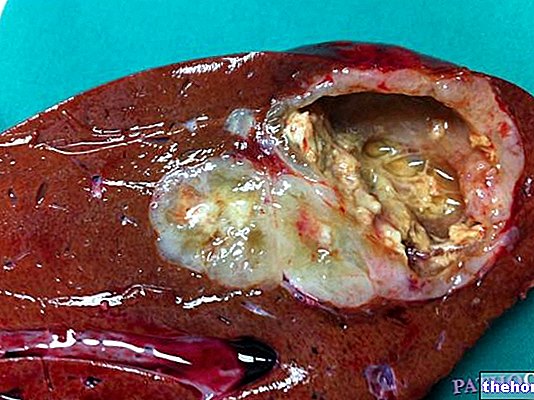
Once the doctor has collected sufficient elements to suspect a thyroid disease, he can complete the evaluation with one or more instrumental tests, such as ultrasound, scintigraphy and needle aspiration. The "basic" instrumental investigation is thyroid ultrasound, useful for examining the morphology and structure of the thyroid. This ultrasound method can provide detailed information on the volume of the gland and on the presence of any nodules or inflammatory processes.
Thyroid scintigraphy with radioactive iodine, on the other hand, is based on the fact that iodine is an essential component of thyroid hormones: by administering, therefore, a small amount of low emission and rapid decaying radioactive substances, it is possible to evaluate the functionality of the thyroid. Thyroid scintigraphy can reveal areas of greater "uptake" of the radioactive iodate tracer and provide a detailed map of the gland by identifying hyperactive nodules.
Finally, needle aspiration or needle biopsy under local anesthesia consists in taking tissue from the thyroid gland through a puncture in the neck, to be subjected to the subsequent histological examination. The method is simple and accurate: in particular, it allows the examination of a lump when it is judged to be "suspicious" and could therefore have a "malignant origin.
The treatment of hyperthyroidism varies according to the cause that induced it and can be substantially pharmacological, radiometabolic or surgical. The goals of these therapeutic approaches are twofold: to control the symptoms and, when possible, to treat the underlying causes.
In most cases, the first choice therapy is represented by thyrostatic drugs, such as methimazole, which reduce the synthesis of thyroid hormones. An important side effect of these drugs that block the action of thyroid hormones is the weakening of the immune system, which can lead to greater susceptibility to infections.
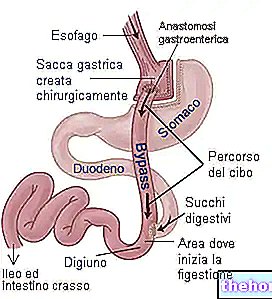
In other cases, radioactive iodine is given or surgery is done. Radioiodine therapy consists in the destruction of overactive thyroid cells through local exposure to radioactive iodine. The drug is administered by mouth and selectively concentrates in the thyroid gland, destroying it under the effect of radiation.
In the case of surgery, however, the doctor removes the thyroid partially or totally, based on what is necessary to control hyperthyroidism. Unfortunately, there is a strong risk of hypothyroidism both in the case of surgery and in the case of radioiodine treatment. In practice, the thyroid - having been partly removed or destroyed by radiation - is unable to secrete adequate amounts of thyroid hormones. In this way, the opposite condition to that of origin is established, ie hypothyroidism. Consequently, the patient will have to resort to replacement therapy by taking synthetic analogues of thyroid hormones by mouth.