Active ingredients: Morniflumato
FLOMAX 700 mg tablets
FLOMAX 350 mg tablets
FLOMAX 350 mg granules for oral suspension
Flomax package inserts are available for pack sizes: - FLOMAX 700 mg tablets, FLOMAX 350 mg tablets, FLOMAX 350 mg granules for oral suspension
- FLOMAX CHILDREN 400 mg suppositories
- FLOMAX ADULTS 700 mg suppositories
Indications Why is Flomax used? What is it for?
This medicine contains the active ingredient morniflumato and belongs to a class of medicines called NSAIDs (non-steroidal anti-inflammatory drugs) that work against pain, fever and inflammation.
FLOMAX is used:
in ADULTS to reduce inflammation, whether or not associated with pain and / or fever, in case of inflammation:
- of the ear (otitis), of the nasal cavities as a whole (sinusitis), of the tonsils (tonsillitis), of the mouth and throat (pharyngitis, laryngitis);
- of the trachea (tracheitis), of the bronchi (bronchitis);
- bladder (cystitis), urethra (urethritis), vagina (vaginitis), prostate (prostatitis), ovaries and fallopian tubes (adnexitis);
- of the bones and joints (osteo-articular system);
in CHILDREN to reduce pain associated with inflammation of the ear (otitis), of the nasal cavities as a whole (sinusitis), of the tonsils (tonsillitis), of the mouth and throat.
Contraindications When Flomax should not be used
Do not take FLOMAX:
- if you are allergic to the active substance or any of the other ingredients of this medicine (listed in section 6);
- if you have had allergy or asthma after taking other NSAIDs such as acetylsalicylic acid known as aspirin;
- if you have a "stomach and / or duodenal ulcer (gastroduodenal);
- if you have had two or more distinct episodes of stomach or bowel ulcer or bleeding (including blood in vomiting or bowel movements or black tarry stools);
- if you have ever had a single episode of stomach or bowel ulcer, perforation or bleeding caused by taking medications;
- if you have severe liver, kidney or heart problems;
- after the sixth month of pregnancy.
Flomax is contraindicated in infants less than six months of age and in infants with a history of rectal inflammation (rectitis), rectal bleeding or ulcer.
Do not take Flomax granules for oral suspension if you have phenylketonuria.
Precautions for use What you need to know before taking Flomax
Talk to your doctor or pharmacist before taking Flomax if:
- you are taking other NSAIDs;
- have had stomach or intestinal disorders, such as ulcer or bleeding, stomach hernia (hiatus), Crohn's disease, ulcerative colitis;
- you are taking medicines that may increase the risk of ulcers and bleeding (see section "Other medicines and Flomax");
- you are elderly or feel very weak (debilitated) or have a low body weight, as you are more likely to develop side effects;
- have asthma associated with chronic inflammation of the nose or nasal passages as a whole (sinusitis) and / or nasal polyps
- have chickenpox, as NSAIDs may worsen the severity of the skin lesions it causes.
- you must undergo urine tests that detect the presence of drugs such as marijuana and hashish, as this medicine can give positive results even in the absence of these substances.
In particular, consult your doctor carefully if:
- has reduced kidney function;
- she recently underwent surgery that caused her a lot of blood loss;
- have liver problems;
- have or have had problems with your heart or blood circulation, such as stroke, heart attack or heart failure or are at risk for these conditions (for example if you have high blood pressure, diabetes or increased triglycerides or smoke), as medicines such as FLOMAX they may be associated with a small increased risk of heart attack (myocardial infarction) or stroke.
IN ALL THESE CASES, THE DOCTOR WILL ASSESS THE NEED TO CARRY OUT CHECK-OUT EXAMINATIONS.
PAY ATTENTION, as during treatment with all NSAIDs:
- Bleeding, ulceration or perforation of the stomach or intestines, which can be fatal, has been reported at any time, with or without warning symptoms, including in patients without previous severe stomach or bowel (gastrointestinal) problems (see section 4.8);
- Although very rarely, severe skin reactions, some of them fatal, have been reported, manifesting as redness, blistering and exfoliation (eg exfoliative dermatitis, Stevens-Johnson syndrome and toxic epidermal necrolysis). In the early stages of therapy, patients appear to be at higher risk: these reactions occur in most cases within the first month of treatment (see section 4.8);
- signs of an infection can be masked.
The risk of having side effects increases with high doses and prolonged treatments. Do not exceed the dose of FLOMAX and do not take it for long periods; always follow your doctor's instructions carefully.
SUSPEND your treatment and contact your doctor if:
- notice any symptoms affecting the stomach and intestines (gastrointestinal), especially if they are bleeding;
- a skin rash, mucosal lesions or any other sign of an allergic reaction (eg redness, itching, swelling of the face and throat, abrupt drop in blood pressure) appear.
Children and adolescents
FLOMAX should be administered in cases of real need and under the direct supervision of the doctor as children and adolescents are more likely to develop side effects with this medicine. In particular, children between 6 and 12 months have a high risk of serious skin side effects.
Interactions Which drugs or foods may change the effect of Flomax
Tell your doctor or pharmacist if you are taking, have recently taken or might take any other medicines, as some medicines can interact with FLOMAX or increase the risk of adverse events, even serious ones.
In particular, you should tell your doctor if you are taking:
- steroidal anti-inflammatory drugs (corticosteroids);
- blood-thinning drugs (anticoagulants and antiplatelet agents), eg warfarin, ticlopidine, clopidogrel, acetylsalicylic acid (known as aspirin) and other NSAIDs, tirofiban, eptifibatide, abciximab, iloprost and heparin;
- diuretics and drugs against high blood pressure (hypertension) such as: ACE inhibitors, beta-blockers, angiotensin II antagonists;
- drugs called "selective serotonin reuptake inhibitors" (SSRIs), used as antidepressants;
- lithium, used in depression;
- methotrexate, used in the treatment of cancer and for certain types of diseases of the immune system, for example rheumatoid arthritis;
- cyclosporine and tacrolimus, drugs that reduce the immune defenses;
- trimethoprim, antibiotic drug;
- potassium salts.
Warnings It is important to know that:
Pregnancy, breastfeeding and fertility
If you are pregnant or breast-feeding, think you may be pregnant or are planning to have a baby, ask your doctor or pharmacist for advice before taking this medicine.
Flomax is contraindicated after the sixth month of pregnancy (see section 4.3). Flomax is not recommended during the first 6 months of pregnancy, except in cases of real need and under the direct supervision of the doctor.
If you are breast-feeding, stop breast-feeding as a precaution while taking Flomax.
- This medicine can impair fertility. This effect is reversible upon discontinuation of the drug.
Driving and using machines
Like other NSAIDs, this medicine may cause dizziness, tiredness and decreased reflexes. Take care before driving or using machines.
FLOMAX tablets contain lactose: if you have been told by your doctor that you have an intolerance to some sugars, contact your doctor before taking this medicine.
FLOMAX granules contains
- sucrose: if you have been told by your doctor that you have an intolerance to some sugars, contact your doctor before taking this medicine;
- sorbitol: if you have been told by your doctor that you have an intolerance to some sugars, contact your doctor before taking this medicine;
- aspartame: this medicine contains a source of phenylalanine. It can be harmful to you if you have phenylketonuria;
- yellow orange S (E 110): may cause allergic reactions.
Dose, Method and Time of Administration How to use Flomax: Posology
Always take this medicine exactly as your doctor has told you, who will tell you the correct dose, based on your disease, and the duration of treatment. If in doubt, consult your doctor or pharmacist.
Adults
1 tablet of FLOMAX 700 mg, 2 times a day
or
2 tablets or 2 sachets of FLOMAX 350 mg, 2 times a day.
Elderly (over 65 years)
1 tablet or 1 sachet of FLOMAX 350 mg, 2-3 times a day, unless otherwise indicated by the doctor.
Your doctor will determine if a dosage reduction is necessary.
Children (over 6 months of age) and adolescents
Children up to 4 years of age (10-15 kg) 1⁄2 sachet of FLOMAX 350 mg, once a day.
Children from 4 to 8 years of age (15-25 kg) 1⁄2 sachet of FLOMAX 350 mg, 2 times a day.
Children and adolescents from 8 to 14 years of age (25-45 kg) 1 tablet or 1 sachet of FLOMAX 350 mg, 2 times a day.
Since the dose of FLOMAX in children depends on body weight, the doctor may prescribe different dosages than indicated.
In children, the duration of treatment with FLOMAX should not exceed 4-5 days.
Method of administration
Take FLOMAX by mouth (orally) and on a full stomach.
The sachet of FLOMAX granules is divided into two parts:
- if you need to take the full dose, open the sachet along the line marked "full dose";
- to take 1⁄2 dose, open the sachet along the line marked "half dose".
Overdose What to do if you have taken too much Flomax
If you take more FLOMAX than you should
You may experience abdominal pain (gastrointestinal irritation), sleepiness, headache. If you are taking large doses of FLOMAX, notify your doctor immediately or go to the nearest hospital, as appropriate measures may be necessary (e.g. charcoal, gastric lavage).
If you forget to take FLOMAX
Do not take a double dose to make up for a forgotten dose.
Side Effects What are the side effects of Flomax
Like all medicines, this medicine can cause side effects, although not everybody gets them.
Stop taking FLOMAX immediately and see your doctor if you have any of the following conditions:
- severe allergic reactions such as: swelling (angioedema) of the face, eyes, lips, throat with difficulty in breathing, sudden drop in blood pressure (anaphylactic shock);
- severe breathing difficulties (asthma attacks);
- severe stomach problems, heartburn or abdominal pain due to ulcer of the stomach or duodenum (peptic) or abdomen;
- sudden violent pain in the pit of the stomach (ulcer perforation);
- vomiting containing blood (haematemesis) or black stools (melaena), associated with bleeding from the stomach or intestines (gastrointestinal) or abnormal fatigue with reduced urine output (due to invisible bleeding);
- severe skin rashes with redness, blistering and exfoliation (e.g. Steven-Johnson syndrome, toxic epidermal necrolysis).
Other side effects with frequency not known (frequency cannot be estimated from the available data)
- worsening of skin infections caused by chickenpox;
- decrease in platelets (thrombocytopenia), decrease in white blood cells (leukopenia);
- headache and dizziness;
- heart attack (myocardial infarction) or stroke, swelling (edema), high blood pressure (hypertension), inability of the heart to supply adequate blood to the body (insufficiency) of the heart, low blood pressure (hypotension), inflammation of the blood vessels blood (vasculitis);
- nausea, vomiting, diarrhea, gas (flatulence), constipation (constipation), indigestion (dyspepsia), pain in the abdomen, inflammation of the lining of the mouth with ulcers (ulcerative stomatitis), worsening of the inflammation of the colon (colitis) and Crohn's disease, gastritis;
- more or less sudden onset of skin lesions, also following exposure to the sun (photosensitization dermatitis), for example spot or diffuse color changes (rash, purpura, erythema multiforme and dermatitis), hives, itching;
- changes in kidney function (kidney failure) which can cause swelling (edema), loss of protein in the urine, decreased protein in the blood (nephrotic syndrome), inflammation of the kidney (interstitial nephritis), blood in the urine (haematuria) ;
- changes in liver tests;
- changes in tests (false positive) that detect the presence of drugs such as marijuana and hashish;
- fluoride intoxication (fluorosis), especially if FLOMAX is taken in high doses and for several years.
Reporting of side effects
If you get any side effects, talk to your doctor or pharmacist. This includes any possible side effects not listed in this leaflet. You can also report side effects directly via the national reporting system at “http://www.aifa.gov.it/responsabili.” By reporting side effects you can help provide more information on the safety of this medicine.
Expiry and Retention
Keep this medicine out of the sight and reach of children.
Do not use this medicine after the expiry date which is stated on the carton after EXP. The expiry date refers to the last day of that month. This date is intended for the product in intact packaging, correctly stored.
Do not throw any medicines via wastewater or household waste. Ask your pharmacist how to throw away medicines you no longer use. This will help protect the environment.
Composition and pharmaceutical form
What FLOMAX contains
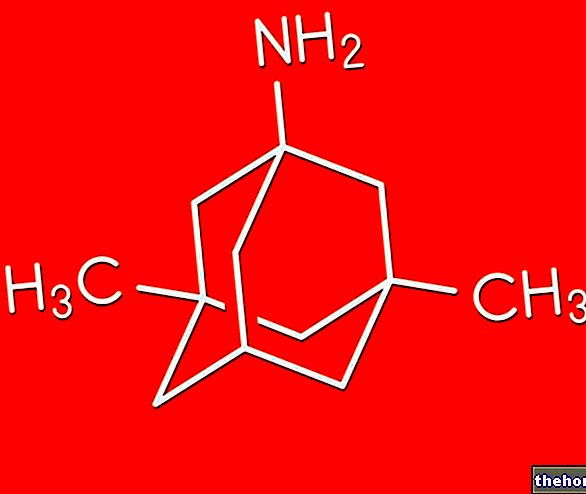
The active ingredient is morniflumato.
Each FLOMAX 700 mg tablet contains: 700 mg of morniflumate.
Each Flomax 350 mg tablet contains 350 mg of morniflumate Each sachet of FLOMAX granules contains: 350 mg of morniflumate.
The other ingredients are:
- FLOMAX tablets: lactose, crospovidone, methylhydroxypropylcellulose, magnesium stearate, sodium laurilsulfate, colloidal hydrated silica.
- FLOMAX granules: sucrose, sorbitol, banana flavor on maltodextrin, fruit flavor, crospovidone, hypromellose, aspartame, ammonium glycyrrhizinate, xanthan gum, polysorbate 20, sodium lauryl sulfate, orange yellow S (E 110).
Description of what FLOMAX looks like and contents of the pack
FLOMAX 700 mg tablets are available in packs of 20 or 30 tablets.
FLOMAX 350 mg tablets are available in packs of 20 tablets.
FLOMAX 350 granules is available in packs of 20 or 30 bipartite sachets.
Source Package Leaflet: AIFA (Italian Medicines Agency). Content published in January 2016. The information present may not be up-to-date.
To have access to the most up-to-date version, it is advisable to access the AIFA (Italian Medicines Agency) website. Disclaimer and useful information.
01.0 NAME OF THE MEDICINAL PRODUCT
FLOMAX
02.0 QUALITATIVE AND QUANTITATIVE COMPOSITION
FLOMAX 700 mg tablets
One tablet contains:
Active ingredient: Morniflumate 700 mg
FLOMAX 350 mg tablets
One tablet contains:
Active ingredient: Morniflumate 350 mg
Excipients with known effect: lactose
FLOMAX 350 mg granules for oral suspension
A bipartite sachet contains:
Active ingredient: Morniflumate 350 mg
Excipients with known effect: sucrose, sorbitol, aspartame and yellow orange S (E 110)
FLOMAX adults 700 mg suppositories
One suppository contains:
Active ingredient: Morniflumate 700 mg
FLOMAX CHILDREN 400 mg suppositories
One suppository contains:
Active ingredient: Morniflumate 400 mg
For the full list of excipients, see section 6.1.
03.0 PHARMACEUTICAL FORM
Tablets, granules, suppositories.
04.0 CLINICAL INFORMATION
04.1 Therapeutic indications
ADULTS. Painful and not painful inflammatory states, also accompanied by fever, affecting the airways (laryngitis, tracheitis, bronchitis), the ENT system (sinusitis, ear infections, tonsillitis, pharyngitis), the urogenital system (cystitis, urethritis, prostatitis, vaginitis, adnexitis) and of the osteoarticular system.
CHILDREN. In children Flomax is indicated in the symptomatic treatment of pain during inflammatory manifestations of the ENT and stomatological system.
04.2 Posology and method of administration
Tablets and granules for oral suspension
Dosage
Adults
1 tablet of Flomax 700 mg, 2 times a day
or
2 tablets or 2 sachets of Flomax 350 mg, 2 times a day.
Elderly (over 65 years)
1 tablet or 1 sachet of Flomax 350 mg, 2-3 times a day.
In the treatment of elderly patients the posology must be carefully established by the doctor who will have to evaluate a possible reduction of the dosages indicated above.
Children (over 6 months of age) and adolescents
Children up to 4 years of age (10-15 kg)
½ sachet of Flomax 350 mg, once a day.
Children from 4 to 8 years of age (15-25 kg)
½ sachet of Flomax 350 mg, 2 times a day.
Children and adolescents from 8 to 14 years of age (25-45 kg)
1 tablet or 1 sachet of Flomax 350 mg, 2 times a day.
In pediatrics, an average daily dose of 17.5 mg / kg body weight is suggested.
Flomax should be administered on a full stomach.
Method of administration (bipartite sachets)
opening the sachet along the line marked "half dose" gives a dose of 175 mg. Opening the sachet along the line marked "full dose" gives a dose of 350 mg.
Flomax should be administered on a full stomach.
Undesirable effects can be minimized with the use of the shortest possible duration of treatment that is needed to control symptoms (see section 4.4).
Suppositories
Adults (Flomax ADULTS 700 mg suppositories)
Two ADULT suppositories (700 mg) per day, one in the morning and one in the evening. The tablet-suppository combination allows a suitable treatment for each case; obviously the dose depends on the clinical picture.
In the treatment of elderly patients the posology must be carefully established by the doctor who will have to evaluate a possible reduction of the dosages indicated above.
Children (Flomax CHILDREN 400 mg suppositories)
Children aged 6 to 12 months: 1 suppository for children per day.
Children over 12 months of age: from 1 to a maximum of 3 suppositories per day according to age and weight. On average, in these cases, the daily dosage is one suppository (285 mg) every 10 kilos of weight for niflumic acid corresponding to 400 mg / 10 kg / day of morniflumato.
Flomax is contraindicated in children under six months of age. In ENT diseases and in stomatology do not exceed 4-5 days of therapy.
The formulation in suppositories, particularly studied for pediatric use, also allows the treatment of patients who cannot feed themselves orally and who in any case have difficulty swallowing and therefore to take the preparation in tablets. Due to the local toxicity, the duration of the rectal administration should be as short as possible.
04.3 Contraindications
Hypersensitivity to the active substance or to any of the excipients listed in section 6.1
Subjects with gastroduodenal ulcer and subjects with hypersensitivity to the active substance or to any of the excipients listed in section 6.1, a history of allergy or "asthma caused by the administration of niflumic acid / morniflumate or substances with similar or closely related activity from a chemical point of view like other NSAIDs and aspirin (see section 4.5).
History of gastrointestinal bleeding or perforation related to previous active treatments or history of recurrent peptic ulcer / haemorrhage (two or more distinct episodes of proven ulceration or bleeding).
Severe hepatic, renal and cardiac insufficiency.
Third trimester of pregnancy (see section 4.6).
• Children under six months of age.
• Children with a history of ulcer, rectitis or rectitis.
The granules (sachets) contain aspartame, therefore it is contraindicated in cases of phenylketonuria.
04.4 Special warnings and appropriate precautions for use
Like other NSAIDs, morniflumate may contribute to an asthma crisis in patients with asthma associated with chronic rhinitis, chronic sinusitis and / or nasal polyposis.
The administration of morniflumate can cause an asthma attack, particularly in certain subjects allergic to acetylsalicylic acid or to an NSAID.
morniflumate may mask the usual signs and symptoms of an infection, therefore it should be used with caution in patients with current infections or in those at risk of infection, even if well controlled.
Exceptionally, chickenpox can cause severe infectious complications of the skin and soft tissues. At the moment it cannot be excluded that NSAIDs may favor the aggravation of these infections. Consequently it is advisable to avoid the use of morniflumate in case of chickenpox (see section 4.8).
During prolonged treatments, periodic blood counts and liver and kidney function indices are recommended.
Precautions for use
Urinary volume and renal function should be closely monitored at the initiation of morniflumate treatment in patients with chronic heart failure, renal or hepatic insufficiency, taking diuretics, who have undergone major surgery resulting in hypovolaemia, and in particular in elderly subjects.
The use of FLOMAX should be avoided in conjunction with NSAIDs, including selective COX-2 inhibitors.
Undesirable effects can be minimized by using the lowest effective dose for the shortest possible duration of treatment needed to control symptoms (see section 4.2 and the paragraphs below on gastrointestinal and cardiovascular risks).
Cardiovascular and cerebrovascular effects
Adequate monitoring and instruction are required in patients with a history of mild to moderate hypertension and / or congestive heart failure as fluid retention and edema have been reported in association with NSAID treatment.
Clinical studies and epidemiological data suggest that the use of some NSAIDs (especially at high doses and for long-term treatment) may be associated with a modest increased risk of arterial thrombotic events (eg, myocardial infarction or stroke). There are insufficient data to exclude a similar risk for morniflumate.
Patients with uncontrolled hypertension, congestive heart failure, established ischemic heart disease, peripheral arterial disease and / or cerebrovascular disease should only be treated with morniflumate after careful consideration. Similar considerations should be made before initiating long-term treatment in patients with risk factors for cardiovascular disease (eg hypertension, hyperlipidaemia, diabetes mellitus, smoking).
Gastrointestinal bleeding, ulceration and perforation:
Gastrointestinal bleeding, ulceration and perforation, which can be fatal, have been reported during treatment with all NSAIDs at any time, with or without warning symptoms or a previous history of serious gastrointestinal events.
The relative risk increases in the elderly, in debilitated subjects, in people with low body weight and in patients who are treated with anticoagulants or antiplatelet agents.
When gastrointestinal bleeding or ulceration occurs in patients taking FLOMAX the treatment should be discontinued.
NSAIDs should be administered with caution and under close medical supervision in patients with a history of gastrointestinal disease (ulcerative colitis, Crohn's disease, hiatal hernia) as these conditions may be exacerbated (see section 4.8 Undesirable effects).
Caution should be exercised in patients taking concomitant medications that may increase the risk of ulceration or bleeding, such as oral corticosteroids, anticoagulants such as warfarin, selective serotonin reuptake inhibitors or antiplatelet agents such as aspirin (see section 4.5).
Elderly: Elderly patients have an increased frequency of adverse reactions to NSAIDs, especially gastrointestinal bleeding and perforation, which can be fatal (see section 4.2).
In the elderly and in patients with a history of ulcer, particularly if complicated with haemorrhage or perforation (see section 4.3), the risk of gastrointestinal bleeding, ulceration or perforation is higher with increased doses of NSAIDs. These patients should start treatment with the lowest available dose. Concomitant use of protective agents (misoprostol or proton pump inhibitors) should be considered for these patients and also for patients taking low dose aspirin or other drugs that may increase the risk of gastrointestinal events (see section 4.5). history of gastrointestinal toxicity, particularly the elderly, should report any unusual gastrointestinal symptoms (especially gastrointestinal bleeding) particularly in the initial stages of treatment.
Skin effects
Serious skin reactions, some of them fatal, including exfoliative dermatitis, Stevens-Johnson syndrome and toxic epidermal necrolysis, have been reported very rarely in association with the use of NSAIDs (see section 4.8). In the early stages of therapy, patients appear to be at higher risk: the onset of the reaction occurs in most cases within the first month of treatment. FLOMAX should be discontinued at the first appearance of skin rash, mucosal lesions or any other signs of hypersensitivity.
Interference with laboratory analyzes
In subjects treated with niflumic acid or morniflumate, false positive results in immunoassay assays have been reported for the presence of cannabinoids in urine (see section 4.8). Therefore, patients treated with niflumic acid or morniflumate, or patients who have recently stopped such treatment, should inform their physician.
Pediatric population
As for other NSAIDs, the use of morniflumate in pediatrics will be carried out after careful evaluation of the risk-benefit ratio for each individual patient.
In the treatment of pediatric patients it is advisable to strictly adhere to the recommended posology (see section 4.2), avoiding therapeutic combinations that may increase the risk of any adverse reactions.
Literature data suggest that the use of niflumic acid in children may be associated with an increased risk of severe mucocutaneous reactions.Since children aged between 6 and 12 months appear to be at greater risk of these reactions, the administration of morniflumate in this age group should only take place after a careful evaluation of the risk / benefit ratio in each individual patient.
Flomax Adult 700 mg suppositories should not be used in pediatrics.
The tablets contain lactose: patients with rare hereditary problems of galactose intolerance, lactase deficiency, or glucose-galactose malabsorption should not take this medicine.
The granules (sachets) contain sucrose: patients with rare hereditary problems of fructose intolerance, glucose-galactose malabsorption, or sucrase-isomaltase insufficiency, should not take this medicine; take this into account for administration to diabetic patients and those undergoing low-calorie diets. The granules also contain sorbitol: patients with rare hereditary problems of fructose intolerance should not take this medicine; it can cause stomach problems and diarrhea.
The use of Flomax, like any prostaglandin synthesis and cyclooxygenase inhibitor drug, is not recommended in women planning to become pregnant.
04.5 Interactions with other medicinal products and other forms of interaction
Diuretics, ACE inhibitors and angiotensin II antagonists
NSAIDs may reduce the effect of diuretics and other antihypertensive drugs. In some patients with impaired renal function (eg dehydrated patients or elderly patients with impaired renal function) co-administration of an ACE inhibitor or an angiotensin antagonist II and agents that inhibit the cyclo-oxygenase system can lead to further deterioration of renal function, including possible acute renal failure, usually reversible. These interactions should be considered in patients taking morniflumate concomitantly with ACE inhibitors or angiotensin II antagonists. Therefore, the combination should be administered with caution, especially in elderly patients.
Patients should be adequately hydrated and monitoring of renal function should be considered after initiation of concomitant therapy.
Risk linked to hyperkalaemia
Some medicinal products or therapeutic classes may favor the onset of hyperkalaemia: potassium salts, diuretics, ACE inhibitors (angiotensin converting enzyme), angiotensin II inhibitors, NSAIDs, heparins (both low molecular weight and not fractional), cyclosporine, tacrolimus and trimethoprim.
The onset of hyperkalaemia may depend on the existence of associated factors. This risk increases when there is a combination with the medicinal products mentioned above.
Risk related to the antiplatelet effect
Many substances are involved in interactions due to their antiplatelet properties: aspirin and NSAIDs, ticlopidine and clopidogrel, tirofiban, eptifibatide and abciximab, iloprost.
The use of many antiplatelet agents increases the risk of bleeding as does their combination with heparins, oral anticoagulants and thrombolytics. Such use should be subject to regular clinical and biological monitoring.
Antiplatelet agents and selective serotonin reuptake inhibitors (SSRIs): increased risk of gastrointestinal bleeding (see section 4.4).
Anticoagulants: NSAIDs may enhance the effects of anticoagulants, such as warfarin (see section 4.4).
Corticosteroids: increased risk of gastrointestinal ulceration or bleeding (see section 4.4).
The simultaneous administration of morniflumate with the following products requires close clinical and biological monitoring of the patient.
Combinations not recommended
With other NSAIDs (including acetylsalicylic acid and other salicylates)
There was an increased risk of gastrointestinal ulcers and bleeding (additive synergy).
With other anticoagulants
An increased risk of bleeding (inhibition of platelet function and damage to the gastroduodenal mucosa caused by NSAIDs) has been found.
If this combination cannot be avoided, close clinical and laboratory monitoring of the patient is required.
With heparin in curative doses or in elderly patients
There was an increased risk of bleeding (inhibition of platelet function and irritation of the gastroduodenal mucosa caused by NSAIDs).
If this combination cannot be avoided, close clinical and laboratory monitoring of the patient is required.
NSAIDs should be administered for a few days.
With lithium
Blood lithium levels are increased and toxic concentrations (reduced renal excretion of lithium) may be reached.
Where necessary, blood lithium levels should be closely monitored and the lithium dosage adjusted during combination treatment and after NSAID treatment has been discontinued.
With methotrexate, used at doses above 15 mg per week
There was an increased risk of haematological toxicity caused by methotrexate (anti-inflammatories reduce the renal clearance of methotrexate).
Combinations requiring precautions for use
With diuretics, ACE inhibitors, and angiotensin II inhibitors
Acute renal failure has been reported in patients at risk (elderly and / or dehydrated subjects) due to a decrease in glomerular filtration (NSAIDs inhibit vasodilating prostaglandins).
Rehydrate the patient. Renal function should be monitored at the start of treatment.
With methotrexate used at doses below 15 mg per week
There was an increased risk of haematological toxicity caused by methotrexate (anti-inflammatories reduce the renal clearance of methotrexate).
Blood counts should be checked weekly during the first few weeks of combination treatment.
In case of renal insufficiency (even if mild), and in elderly patients, close monitoring is required.
Combinations that need to be considered
An increased risk of haemorrhage was found with other antiplatelet agents (ticlopidine, clopidogrel, tirofiban, eptifibatide and abciximab, iloprost) and with heparins at prophylactic doses.
With other agents that cause hyperkalaemia (potassium salts, potassium-sparing diuretics, ACE inhibitors (angiotensin converting enzyme), angiotensin II inhibitors, other NSAIDs, heparins (both low molecular weight and unfractionated), ciclosporin, tacrolimus and trimethoprim) there was an increased risk of hyperkalaemia.
With beta blockers (by extrapolation of indomethacin data)
A reduction in the antihypertensive effect has been found (NSAIDs inhibit vasodilating prostaglandins).
With cyclosporine
Risk of potentiation of nephrotoxic effects, particularly in the elderly patient.
04.6 Pregnancy and lactation
Fertility. Cases of secondary non-ovulatory infertility caused by non-rupture of the Graafian follicle have been reported in patients of childbearing age taking long-term prostaglandin synthesis inhibitors.
This infertility is reversible upon discontinuation of treatment.
Pregnancy. Inhibition of prostaglandin synthesis can adversely affect pregnancy and / or embryo / fetal development.
Results of epidemiological studies suggest an increased risk of miscarriage and cardiac malformation and gastroschisis after use of a prostaglandin synthesis inhibitor in early pregnancy. The absolute risk of cardiac malformations increased from less than 1% to approximately 1.5%. The risk has been considered to increase with dose and duration of therapy. In animals, administration of prostaglandin synthesis inhibitors has been shown to cause increased loss of pre- and post-implantation and of embryo-fetal mortality.
In addition, an increased incidence of various malformations, including cardiovascular, has been reported in animals given prostaglandin synthesis inhibitors during the organogenetic period.
During the first and second trimester of pregnancy, FLOMAX should not be administered except in strictly necessary cases.
If FLOMAX is used by a woman attempting to conceive, or during the first and second trimester of pregnancy, the dose and duration of treatment should be kept as low as possible.
During the third trimester of pregnancy, all prostaglandin synthesis inhibitors can expose the fetus to:
• cardiopulmonary toxicity (with premature closure of the arterial duct and pulmonary hypertension);
• renal dysfunction, which can progress to renal failure with oligo-hydroamniosis;
the mother and the newborn, at the end of pregnancy, to:
• possible prolongation of bleeding time, and antiplatelet effect which may occur even at very low doses;
• inhibition of uterine contractions resulting in delayed or prolonged labor
Consequently, FLOMAX is contraindicated during the third trimester of pregnancy.
Feeding time. The concentration of niflumic / morniflumate acid in milk is low. However, as a precaution, breastfeeding should be stopped.
04.7 Effects on ability to drive and use machines
Similarly to other non-steroidal anti-inflammatory drugs, the drug could induce drowsiness or sensory numbness with impairment of activities that require alertness (driving cars, use of machinery, etc.).
The patient should be advised of the possibility of manifestations such as dizziness or drowsiness.
04.8 Undesirable effects
The most commonly observed adverse events with NSAIDs are gastrointestinal in nature. Peptic ulcers, gastrointestinal perforation or haemorrhage, sometimes fatal, may occur, particularly in the elderly (see section 4.4).
Edema, hypertension and heart failure have been reported in association with NSAID treatment.
The frequency of adverse events, listed below in the table, cannot be estimated from the available data, as they have been reported in post-marketing experience.
(*) Increases in dosage and duration of treatment influence the increased frequency of gastrointestinal side effects (see section 4.4).
In case of chickenpox, serious skin infectious complications may occur (see section 4.4).
(**) Clinical studies and epidemiological data suggest that the use of some NSAIDs (especially at high doses and for long-term treatments) may be associated with a modest increase in the risk of arterial thrombotic events (ie myocardial infarction or cerebrovascular accident ; see section 4.4).
Reporting of suspected adverse reactions
Reporting of suspected adverse reactions occurring after authorization of the medicinal product is important as it allows continuous monitoring of the benefit / risk balance of the medicinal product. Healthcare professionals are asked to report any suspected adverse reactions via the national reporting system. "address" www.agenziafarmaco.gov.it/it/responsabili ".
04.9 Overdose
In the event of an overdose with niflumic acid / morniflumate the foreseeable symptoms are: gastrointestinal irritation, drowsiness (5%) and headache. One subject who ingested 7.5 g of niflumic acid showed glomerulonephritis, which resolved without sequelae. In the event of an overdose, symptomatic treatment is indicated, in addition to gastric lavage and administration of activated charcoal (oral forms only).
05.0 PHARMACOLOGICAL PROPERTIES
05.1 Pharmacodynamic properties
Pharmacotherapeutic group: non-steroidal anti-inflammatory. ATC code: M01AX22
FLOMAX is a specialty based on morniflumate, beta-morpholinoethyl ester of 2 [[3- (trifluoro-methyl) -phenyl] -amino] 3-pyridincarboxylic acid.
Morniflumate is a non-steroidal compound with anti-inflammatory, antipyretic and secondarily analgesic activity, characterized by a particularly favorable therapeutic index.
Preclinical studies have shown how morniflumate has a marked anti-inflammatory activity, revealing itself to be active in various experimental models of inflammation, such as carrageenan and nystatin edema in rats and erythema from U.V. in the guinea pig. This activity is comparable to that of niflumic acid and flufenamic acid.
Morniflumate is active in experimentally induced hyperthermia to a comparable or greater extent to other analogous compounds (dipyrone, acetylsalicylic acid and paracetamol).
Even the "analgesic activity, tested by the" Writhing-Test from phenylquinone "in the mouse and the" Randall-Selitto test "in the rat, is equipotent to that of niflumic acid but double compared to that manifested by fluphenamic acid and dipyrone, and significantly higher than that exhibited by acetylsalicylic acid and paracetamol.
In animal studies, the product was found to have no ulcerogenic effect, in fact no gastric lesions were detected in the rat up to doses of the order of 4000 mg / kg, considerably higher than the pharmacologically active doses.
The high gastric tolerability of morniflumate is probably attributed not only to the virtual absence of local physical-chemical irritation on the gastric mucosa but, presumably, also to the lack of inhibition by the drug of the synthesis of prostaglandins with cytoprotective activity (PGI2 and PGE2) .
05.2 Pharmacokinetic properties
Pharmacokinetic studies have shown that the orally administered product is rapidly absorbed as such from the gastrointestinal tract and is subsequently rapidly hydrolyzed into the plasma, releasing the corresponding acid; excretion is rapid, mainly through the renal emunctory, without risks of accumulation in the organism. Also rectally, the morniflumate is rapidly absorbed and immediately hydrolyzed to niflumic acid, reaching the plasma peak after about 5 hours.
05.3 Preclinical safety data
The oral LD50 values were equal to 4300 (M) and 4950 (F) mg / kg in the rat and 4850 (M) and 5400 (F) mg / kg in the mouse.
For repeated oral administration, morniflumate was well tolerated up to doses of 100 mg / kg in rats and 60 mg / kg in dogs for 6 months.
Rectal tolerability was good in the rabbit after one month of treatment.
Furthermore, no carcinogenic, allergenic, sensitizing or immunosuppressive effects were found in animals.
As regards use during pregnancy and lactation, please refer to the information reported in paragraph 4.6 above.
06.0 PHARMACEUTICAL INFORMATION
06.1 Excipients
Tablets: Lactose, Crospovidone, Methylhydroxypropylcellulose, Magnesium stearate, Sodium laurilsulfate, Hydrated colloidal silica.
Granulated: Sucrose, Sorbitol, Banana flavor on maltodextrin, Fruit flavor, Crospovidone, Hypromellose, Aspartame, Ammonium glycyrrhizinate, Xanthan gum, Polysorbate 20, Sodium laurilsulfate, Orange yellow S (E 110).
Suppositories: Solid semisynthetic glycerides.
06.2 Incompatibility
Not known.
06.3 Period of validity
Tablets: 5 years.
Granules, suppositories: 3 years.
The period of validity indicated refers to the product in intact packaging, correctly stored.
06.4 Special precautions for storage
Suppositories: store at a temperature not exceeding 30 ° C.
06.5 Nature of the immediate packaging and contents of the package
Tablets
Internal packaging: PVC / Al blister; external packaging: printed cardboard case.
Box of 20 tablets of 350 mg
Box of 20 tablets of 700 mg
Box of 30 tablets of 700 mg
Granulated
Inner packaging: PE / Al / paper bags; external packaging: printed cardboard case.
Box of 20 bipartite sachets of 350 mg
Box of 30 bipartite sachets of 350 mg
Suppositories
PVC / PE strips, printed cardboard case.
Box of 10 adult suppositories (700 mg)
Box of 10 suppositories for children (400 mg)
Not all pack sizes may be marketed.
06.6 Instructions for use and handling
Unused medicine and waste derived from this medicine must be disposed of in accordance with local regulations.
07.0 MARKETING AUTHORIZATION HOLDER
CHIESI FARMACEUTICI S.p.A., Via Palermo 26 / A - Parma
08.0 MARKETING AUTHORIZATION NUMBER
027244058 FLOMAX 350 mg tablets - 20 tablets
027244060 FLOMAX 700 mg tablets - 20 tablets
027244084 FLOMAX 700 mg tablets - 30 tablets
027244072 FLOMAX 350 mg granules for oral suspension - 20 bipartite sachets
027244096 FLOMAX 350 mg granules for oral suspension - 30 bipartite sachets
027244108 FLOMAX adults 700 mg suppositories - 10 suppositories
027244110 FLOMAX children 400 mg suppositories - 10 suppositories
09.0 DATE OF FIRST AUTHORIZATION OR RENEWAL OF THE AUTHORIZATION
FLOMAX 350 mg tablets - 20 tablets 02/04/1990
FLOMAX 700 mg tablets - 20 tablets 02/04/1990
FLOMAX 700 mg tablets - 30 tablets 29/10/1994
FLOMAX 350 mg granules for oral suspension - 20 bipartite sachets 02/04/1990
FLOMAX 350 mg granules for oral suspension - 30 bipartite sachets 29/10/1994
FLOMAX adults 700 mg suppositories - 10 suppositories 20/05/2002
FLOMAX children 400 mg suppositories - 10 suppositories 20/05/2002
10.0 DATE OF REVISION OF THE TEXT
March 2015