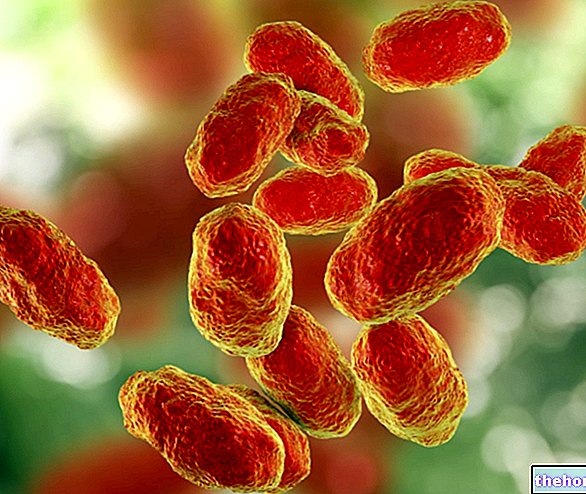
Pseudomonas aeruginosa it is a small rod-shaped bacterium (length of 1.5 - 3 µm and width between 0.5 and 0.8 µm).

In humans it is an opportunistic pathogen, which can occasionally be found in the axillary, inguinal and anogenital skin regions of healthy subjects. Pseudomonas aeruginosa it has been isolated in approximately 10% of human stool samples.
There are numerous virulence factors that determine its pathogenicity:
- the outer lipopolysaccharide layer (LPS) protects Pseudomonas aeruginosa by the phagocytic action of neutrophilic leukocytes, it favors their adhesion to the tissues, and decreases the susceptibility of the microorganism to the bactericidal action of some antibiotics
- the mobility (flagellum) and the presence of pili, fimbriae and adhesins, in addition to the LPS itself, facilitate its adhesion to the tissues and mucus (the infection by Pseudomonas aeruginosa respiratory is common in patients with cystic fibrosis)
- toxins of various kinds (elastase, collagenase, protease, lipase) produced by the bacterium destroy the surrounding tissue, favoring the progression of the microorganism
- other protein toxins (exotoxin A, cytotoxin, hemolysins, pyocyanin) are involved in virulence mechanisms
Pseudomonas aeruginosa it is above all an opportunistic nosocomial pathogen; it therefore produces infections especially in hospitalized patients, preferring those who are debilitated, immunocompromised or undergoing urethral catheterization, mechanical ventilation, lumbar punctures and intravenous perfusions.
Infections with Pseudomonas aeruginosa they are quite rare. In the healthy child, diseases from Pseudomonas aeruginosa are limited to local infectious processes at the site of attack: external otitis, urinary infections, dermatitis (intertrigo). In subjects immunocompromised due to metabolic or haematological diseases, tumors, prolonged antibiotic therapy or chemotherapy, the " Pseudomonas aeruginosa it can become disseminated and cause, for example, pneumonia, endocarditis, peritonitis, meningitis and severe septicemia.
Diseases caused by pseudomonas aeruginosa
Infections from Pseudomonas aeruginosa they can occur in many anatomical locations, such as skin, subcutaneous tissues, bones, ears, eyes, urinary tract, and heart valves. Location varies according to doorway and patient vulnerability. Symptoms of Pseudomonas aeruginosa they therefore depend on the body site affected by the infectious process.
District concerned
Wounds, pressure ulcers, intertrigo, burns, surgical trauma, intravenous injection infections, haemorrhagic skin necrosis or gangrenous ecthyma
Ear
External otitis of swimmers, internal otitis of diabetics
Eye
Corneal ulcer, traumatic abrasion or surgical trauma, such as those suffered during cataract surgery
Respiratory System
Tracheobronchitis, Bronchopneumonia, Necrotizing pneumonia from contaminated respirators, endotracheal intubation infections, respiratory distress syndrome in adults, infection in patients with cystic fibrosis
Urogenital system
Urinary tract infections resulting from catheter application or irrigation
Digestive system
Diarrhea in children (Shanghai fever), cholera-like diarrhea, typhlitis in leukemics, rectal abscesses in cancer patients
Circulatory system
Methemoglobinemia, Septicemia, Endocarditis (quite rare, more common in drug addicts who take intravenous drugs).
Nervous system
Treatment and therapy
Therapeutic interventions also depend on the site in which Pseudomonas aerugnosa produced infection. For example, in case of skin involvement, it is possible to resort to irrigations of 1% acetic acid or to the topical application of antibacterial agents such as polymyxin B or colistin. The correct hygiene of the affected skin areas is of particular importance: any necrotic tissue must be eliminated and the abscesses drained, while in the hospital it is essential to carefully clean and disinfect medical equipment.
If systemic antibiotic therapy is required, tobramycin or gentamicin is generally used.In case of resistance to these drugs, amikacin can be used as an alternative according to medical indications.
The Pseudomonas aeruginosa is assuming significant clinical importance due to its multiple resistance to various antibiotics, so it is necessary to carry out sensitivity tests in vitro (antibiogram) on the strain isolated from the clinical sample.
- Among the penicillins active against Pseudomonas aeruginosa remember piperacillin, ticarcillin and mezlocillin.
- Among the cephalosporins active against Pseudomonas aeruginosa remember: ceftazidime and cefoperazone (also known as third generation cephalosporins antipseudomonas).
- Among the fourth generation parenteral cephalosporins active against Pseudomonas aeruginosa remember: cefepime, imipenem, metropenem and aztreonam.
- Many aminoglycosides active against Pseudomonas aeruginosa: tobramycin, amikacin and gentamicin.
- Among the fuloroquinolins, ciprofloxacin appears to be the most active against the mycorganism; the antibiotic action of levofloxacin is slightly lower, while the other fluoroquinolones are not at all or scarcely effective.