Tests for the molecular diagnosis of HPV infections have been available for several years now, during which an enormous amount of data has been collected regarding the reliability and diagnostic usefulness of these investigations. these tests in cervical cancer screening programs.
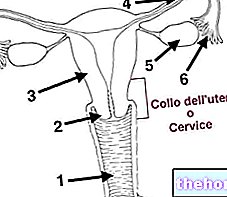
From the "operational" point of view, the "molecular investigation is carried out in the same way as the pap test: the patient must undergo the removal of cervical material using special instruments. For this reason, and also for the best diagnostic significance, an HPV Positive DNA test is followed by conventional cytology (pap smear).
In general, the HPV tests performed in association with the pap test allow to:
- identify a greater number of papillomavirus infections than those detected with the pap test alone, which in some circumstances can miss up to one in ten at risk (false negative result)
- better quantify the risk of developing cervical cancer, thanks to the possibility of identifying serotypes with high oncogenic risk
- to strengthen, in case of negativity, the diagnostic value of a negative pap smear, classifying the patient as at low risk with possible temporal thinning of the subsequent control investigations. In other words, a negative HPV test gives greater guarantees that the disease is not present and that it will not be in the short period of time.
- add important diagnostic information to pap-tests with an uncertain outcome, making it possible to distinguish positive patients from the virus from negative ones, directing them in case of further positivity to colposcopy.
Regarding the use of the HPV-test as a primary screening tool instead of the pap test, we can reasonably state that:
- the search for HPV with high oncogenic risk (HR-HPV) has a greater sensitivity than the pap smear, but is burdened by a lower specificity, especially in young women; therefore, given the frequent reversibility of the infection, a positive result would risk subjecting a greater number of young patients to unnecessary apprehensions, investigations and treatments
- in women over the age of 30 the HPV test acquires specificity and can therefore be used as a primary screening tool starting from 30/35 years, with cytology (pap test) performed only in the case of a positive HPV test.
In general - gathering the opinion of the various associations and guidelines, which are constantly updated - we can reasonably state that:
- the performance of the HPV DNA test as the primary screening tool is NOT indicated in women under the age of 30, given the high incidence and reversibility of the infection in this age group;
- Within three years from the beginning of sexual activity but in any case not before the age of 21, or from the age of 25 according to other sources, it is advisable to undergo a pap test every 3 years (the old sources, however, spoke of more frequent checks , every 1-2 years); in this regard, it is important to underline that also women subjected to HPV vaccination MUST undertake PAP-test screening.
- in women under the age of 30 who have abnormal pap smear results of the type "atypical squamous cells of undetermined significance", it is possible to use the "HPV test as a follow-up investigation to monitor the evolution of the situation and establish the" whether or not to undergo colposcopy
- starting from 30/35 years, pap smear screening every 3 years can be replaced by HPV test every 5 years.
- in women over the age of 30/35 years the joint execution of cytological examination and HPV test is indicated only in case of positive PAP-test (or vice versa).
- If you opt for the pap smear as a screening method, in case of negative result and in the absence of further risk factors (HIV, sexual promiscuity, previous history of cervical cancer, smoking ...), the investigation should be repeated every 3 years; on the other hand, if you opt for the HPV test, in the event of a negative result and in the absence of further risk factors, the investigation should be repeated every 5 years → stop performing it from 65 years of age.

The graph summarizes the concepts expressed in the course of the article: note the peak incidence of cervical HPV infections between the ages of 15 and 25, and the increase in the incidence of precancerous and neoplastic lesions after 25 years. age, expression both of the organism's remarkable ability to eradicate infections, and of the latency between HPV infection and the onset of cervical cancer; this last point, in particular, allows secondary prevention through screening
Exam execution and preparation
As anticipated, to perform the HPV test, a sample of cells is taken from the cervix, exactly as for a normal Pap test (see: how to perform a pap test).
In view of the examination, the patient is required to strictly comply with these rules:
undergo the HPV test at least 5 days before your period or at least 5 days after it stops.
refrain from sexual intercourse for at least two days
avoid the application of creams, pessaries and vaginal irrigators in the 5 days preceding the examination
Other articles on "When to get the pap smear and the" HPV test "
- Pap test: when to do it?
- PAP test
- Pap smear and prevention
- Pap test results: how to read and interpret them
- Colposcopy
- Colposcopy results: read and interpret them