In reality, as shown in the image, the two terms refer to two distinct anatomical regions:
- the mandible forms the lower scaffolding of the mouth. It houses the lower teeth in the alveolar arch and is the only mobile part of the face.
- the jaw, on the other hand, forms the upper scaffolding of the mouth and houses the upper dental arch. Unlike the mandible, the maxilla is a fixed bone, so it does not move with the opening and closing of the mouth.
The fact that the mandible is often referred to as the lower jaw, and that the maxilla is often referred to as the upper jaw, fuels the confusion between the two terms. Altogether the two bones are also referred to as maxillary bones.
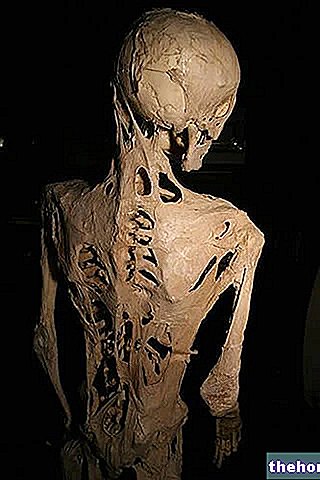
of the maxilla is a serious disease that affects one or both jaw bones (mandible and maxilla).
Osteonecrosis literally means "bone death." It is therefore easy to understand how mandibular osteonecrosis leads to infectious complications (osteomyelitis), with chronic ulceration of the oral mucosa and exposure of the underlying necrotic bone.
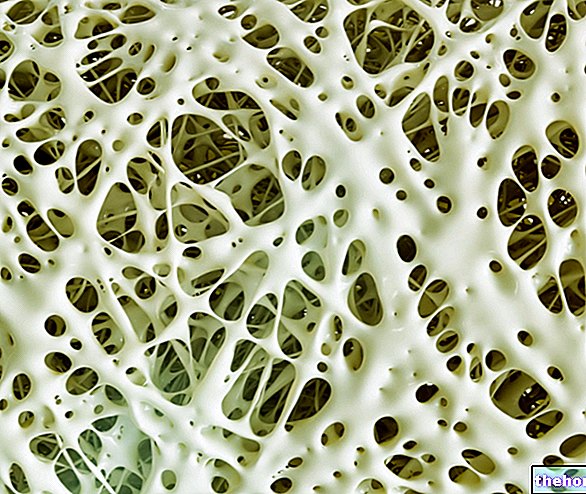
Recently, the use of bisphosphonates (or bisphosphonates) has been included among the possible causes of osteonecrosis of the jaw. These drugs - including alendronate, risedronate, ibandronate and zoledronate - act as inhibitors of bone resorption. For this reason they are commonly prescribed in the prevention and treatment of osteopenia and osteporosis.
However, the greatest risks are borne by those patients who take bisphosphonates to treat some bone complications of cancer (lytic bone metastases). In these cases, in fact, the dosages used are much higher.
Although the risk of osteonecrosis of the jaw - related to the use of low-dose bisphosphonates for the treatment and prevention of osteoporosis - is still unclear, it is advisable to inform your dentist during (or rather before starting) therapy with these. drugs, especially in view of invasive dental interventions such as dental implants.
A "careful oral hygiene, assisted by periodic dental visits, is very important; in fact, the risk of osteonecrosis of the jaw associated with the use of bisphosphonates seems greater in patients with poor oral hygiene, with periodontal diseases or in case of invasive dental care during the treatment.
male are well imprinted in the common imagination, few know that in women the signs of a heart attack are often more subtle.
In the movies, for example, heart attacks fall to the ground panting in severe chest pain. In fact, the sensation of chest tightness and constriction (as if a boulder weighed on the chest or as if it were squeezed in a vise) represents the most common symptom of heart attack, in both sexes, but in reality the symptoms of heart attack they can also be quite nuanced.
Especially in women, but also in men, the symptoms of a heart attack can be limited to widespread pain in the back, jaws or pit of the stomach, with nausea, fatigue, indigestion and vomiting. Symptoms that are not normally given too much weight, thinking they are due to a trivial flu or gastroesophageal reflux problems.
SIGNS AND SYMPTOMS OF HEART ATTACK IN WOMEN
As for men, even in women the most characteristic symptom of heart attack is chest pain, which can be a simple discomfort or very intense pain.
Women, however, are somewhat more likely than men to experience some of the other less common symptoms of heart attack, particularly shortness of breath, nausea, vomiting, and back or jaw pain.
Therefore, in the unfortunate circumstance in which these symptoms are felt, it is good to immediately alert the health services; even when the symptoms have subsided, the heart attack could be very serious.
- Sense of pressure or pain in the center of the chest. This symptom lasts more than a few minutes, or comes and goes.
- Pain or discomfort in one or both arms, back, neck, jaw or stomach.
- Shortness of breath, with or without chest pain.
- Cold sweats, nausea or dizziness.