The follicular phase (or proliferative phase) is the first phase of the ovarian cycle: it begins with the first day of the menstrual cycle and ends with ovulation. The duration of this phase is on average 14 days, but it can also vary significantly from woman to woman. per woman and from cycle to cycle; vice versa, the next phase of the menstrual cycle, the luteal phase, is more stable in terms of duration, which is always equivalent to 14 days.
Inside the ovaries there are numerous follicles at different stages of development. Most of these are in a phase defined as primordial (immature), but some of them begin to develop into preovulatory follicles, each proceeding independently of the others.
The fundamental function of the follicles is to constitute the support for the oocytes, the egg cells enclosed within them.

Contrary to male spermatogenesis (which can last indefinitely), folliculogenesis ends when menopause is reached: the follicles in the ovaries are no longer sensitive to the hormonal signals that previously induced the follicular phase.
The follicular phase has two critical points beyond which the development of the follicle cannot proceed unless there are highly specific changes both in the structure of the follicle itself and in the composition of the surrounding environment. These critical points divide the follicular phase into three sub-phases different from physiological point of view: pre-antral phase, antral phase and pre-ovulatory phase.
Preantral phase
The pre-antral phase has a variable duration, but is generally thought to last from 3 to 5 days.
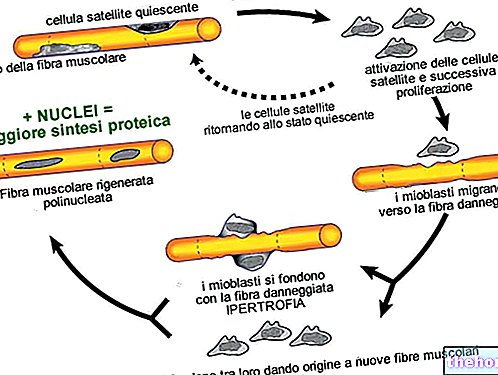
- When a follicle develops, follicular cells proliferate forming multiple layers around the oocyte and differentiate into granulosa cells. The follicle from primordial thus becomes a primary follicle.
- During the pre-antral stage, the cells of the granulosa begin to secrete large quantities of glycoproteins which will form a thick membrane called zona pellucida around the oocyte and the granulosa. The exchange of metabolites with the oocyte is ensured by the communicating junctions located in the extensions. cytoplasmic between the oocyte and the surrounding granulosa cells.
- Some specific connective tissue cells (ovarian stroma) differentiate to form the outer layer of theca cells. In this matrix, two layers are soon distinguished: an internal case (full of vessels, glandular) and an external case.
- The last modification of the follicle occurs towards the end of the pre-antral phase and consists in the appearance on the membranes of both types of follicular cells of gonadotropin receptors:
- luteinizing hormone (LH) receptors on thecal cells
- follicle-stimulating hormone (FSH) receptors on granulosa cells.
The presence of these receptors is essential for the continuation of ovogenesis, as the transition to the next antral phase can only occur in the presence of gonadotropic hormones. Some follicles do not pass this stage and undergo atresia (degeneration with consequent death of the oocyte ).
Antral phase
The preantral follicles enter this stage if there is an adequate concentration of luteinizing hormone (LH) and follicle-stimulating hormone (FSH) in the bloodstream, and if the follicle has acquired a sufficient number of receptors for these hormones.
The follicles that continue their development form a fluid-filled cavity called the antrum, which is constantly expanding (early antral stage). At this point the follicles are called secondary follicles; in a typical ovarian cycle about 15-20 follicles enter this stage of development. After about seven days, one of these follicles (dominant follicle) is selected to complete its development, while the remaining secondary follicles will undergo atresia.
The change in the structure, associated with the formation of the antrum, corresponds to a functional transformation of the follicle which becomes a real endocrine gland, responsible for producing increasing quantities of androgens (androstenedione and testosterone), estrogens (especially estradiol) and, in a next stage, progestogens.
As explained, follicular growth and development are promoted by both FSH and estrogen secreted by the follicle itself. Plasma levels of FSH gradually decrease during the follicular phase. This tends to cause decreased estrogen secretion. dominant follicle depends on its ability to produce adequate levels of estrogen in the face of falling FSH levels.

The dominant follicle continues its development in the late antral stage: some cells of the granulosa surrounding the oocyte form the cumulus oophore, a small cord of cells that attacks the oocyte and the corona radiata (consisting of layers of granulosa cells surrounding the oocyte) to the follicle wall, now called Graafian follicle.

The duration of the antral phase is generally 8-12 days.
Pre-ovulatory phase
To enter the pre-ovulatory phase, the mature antral follicle must find an adequate concentration of FSH and LH in the surrounding environment, so that it does not undergo atresia. Blood levels of gonadotropins are much higher than at normal values: there is a pre-ovulatory peak in the concentration of FSH and a real surge of LH (defined as LH-surge).
The phase is defined pre-ovulatory as it precedes the ovulation event just a little (lasts about 37 hours). This stage is defined as the phase of maturation or rupture of the germinal vesicle, as we basically witness the resumption of meiosis with the detachment of the secondary oocyte from the wall, which is free to float in the antral fluid, together with the radial crown that covers it. In this third stage of the follicular phase of the ovarian cycle, the pre-ovulatory follicle considerably increases its volume.
Hormonal regulation of the follicular phase

During the follicular phase of the ovarian cycle, the growth and differentiation of follicles are processes subjected to a delicate and precise balance between the levels of circulating hormones and the production of their receptors in the follicular cells. If the levels of circulating hormones and the appearance of their receptors coincide, then follicular development can continue; vice versa, if this condition is not reached, the follicles undergo degeneration and the formation of atretic bodies of the ovary.
Hormonal regulation is a fundamental control mechanism of the ovarian cycle.
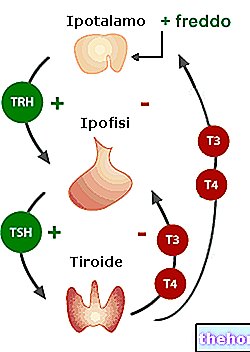
There are five hormones that participate in the complex positive and negative feedback process to regulate folliculogenesis:
- gonadotropin-releasing hormone (GnRH) secreted by the hypothalamus
- follicle-stimulating hormone (FSH)
- luteinizing hormone (LH)
- estrogen
- progesterone
The hormones produced by the pituitary gland (FSH and LH) and the hormones produced by the ovary (estrogen and progesterone) have antagonistic effects (negative feedback control).
At the same time, to transform the continuous production of primary follicles into the periodic phenomenon of ovulation, at least two positive feedback mechanisms must intervene:
- antral phase: exponential production of estrogen;
- preovulatory phase: exponential production of FSH and LH.