Generality
The term "contraceptives" refers to the set of drugs and devices used to prevent the onset of pregnancy.
![]()
- Hormonal methods of contraception, including oral contraceptives, injectable contraceptives, the contraceptive patch and some types of intrauterine devices;
- Barrier contraceptive methods, including condoms and other types of intrauterine devices.
Below, these contraceptive methods will be briefly described, with a particular focus on hormonal-type contraceptives.
Oral contraceptives
As mentioned, oral contraceptives fall into the category of hormonal type contraceptives.
In turn, oral contraceptives can be divided into two groups:
- Oral contraceptives in combination;
- Oral contraceptives progestin (often referred to as a "minipill").
As you can easily guess, combined oral contraceptives are drugs that contain a combination of several active ingredients. More specifically, they contain a combination of an estrogenic-type active ingredient and a progestin-type active ingredient.
Conversely, progestin oral contraceptives do not contain the estrogenic component, but only the progestogen component.
Active ingredients such as ethinylestradiol (Ginoden®, Loette®, Arianna®, Belara®, Yasmin®, Yasminelle®), estradiol (Zoely®), levonorgestrel (Loette®, Egogyn®), gestodene (Ginoden®, Arianna®, Milavane®), drospirenone (Yasmin®, Yasminelle®) and desogestrel (Cerazette®, Mercilon®, Minulet®).
Mechanism of action
The estrogen contained within oral contraceptives exerts its contraceptive action by suppressing the release of follicle stimulating hormone (or FSH), thus preventing the formation of a dominant follicle during the follicular phase of the menstrual cycle.
The dominant follicle, in fact, is responsible for the synthesis of estradiol which, in turn, sends a negative feedback signal to the hypothalamus. All this results in an inhibition of the secretion of gonadotropins, which thus prevents the maturation of other follicles. Therefore, estrogen is able to prevent this series of events, but not only. In fact, the estrogenic component is also responsible for maintaining the stability of the endometrium.
The progestin, on the other hand, exerts its contraceptive action by blocking ovulation by inhibiting the synthesis of luteinizing hormone (or LH) in the middle of the menstrual cycle. Furthermore, the progestin component is also able to induce a thickening of the cervical mucosa, which hinders the passage of sperm into the endometrial cavity and is also capable of transforming the endometrium into a hostile environment for the implantation of the embryo.
Side effects
The main side effects produced by the estrogenic component are those of the cardiovascular type; in fact, estrogen increases the risk of developing venous thromboembolism, acute myocardial infarction and stroke.
The main undesirable effects caused by the progestin component, on the other hand, consist in the "increase in blood levels of triglycerides and in the decrease in serum HDL levels. Therefore, if the so-called minipill is used, the risk of onset of cardiovascular effects is greatly reduced. since there is no estrogen present.
In any case, for more information regarding the aforementioned side effects, we recommend reading the dedicated articles "Birth control pills and blood pressure" and "Birth control pills and cholesterol".
Transdermal contraceptive patches
Even the transdermal patches with contraceptive action fall into the category of hormonal contraceptives, but unlike oral contraceptives, transdermal patches are pharmaceutical formulations with a long duration of action. In fact, these patches, once applied, slowly release the active ingredients of estrogenic and progestin type.
More specifically, these active ingredients are generally ethinyl estradiol and norelgestromin (Evra®).
The patch must be applied to an arm, buttock or abdomen and must be replaced once a week (always on the same day) for three consecutive weeks. At the end of these three weeks, an interruption must be observed. one week to allow for withdrawal bleeding.
Furthermore, it should be remembered that - although well tolerated - the contraceptive patch may not be effective in patients with a body weight greater than 90 kg.
Mechanism of action
Since these are hormonal contraceptives, the mechanism of action by which the active ingredients contained in the transdermal patches exercise their contraceptive activity is the same as described for the aforementioned oral contraceptives.
Side effects
The main side effects that can occur following the use of transdermal contraceptives are: nausea, headache, abdominal pain, breast pain and irritation at the site where the patch is applied.
Injectable contraceptives
In some cases, the doctor may decide to resort to long-term contraception through the use of injectable contraceptives, which can be either in combination or of the progestin type.
More specifically, both pharmaceutical formulations containing a combination of medroxyprogesterone acetate and estradiol cypionate, and pharmaceutical formulations containing only the progestogen-type active ingredient, such as medroxyprogesterone acetate (Perlessa®, Sayanaject) are commercially available.
The mechanism of action of these drugs is similar to that described for oral contraceptives.
Even the side effects are similar to those deriving from the use of oral contraceptives and consist of: headache, breast tenderness, decreased libido, weight gain.
However, in addition to the aforementioned side effects, injectable progestogen contraceptives may also increase the risk of irregular and profuse bleeding, amenorrhea and infertility which can last long after the last injection.
Implantable contraceptives
To this particular category of contraceptives belong both surgically implantable contraceptives (such as hormonal sticks), and some types of intrauterine devices (or IUD, from the "English" Intra-Uterine Device "), such as the hormonal coil that releases a contraceptive into the body. progestin and like the copper-coated IUD.
In particular, this last type of device carries out the contraceptive activity through a mechanical irritation of the endometrium. In this way, an unfavorable inflammatory environment for sperm and ova is created, which does not allow the embryo to implant.
All these devices must be implanted (in the case of sticks) or inserted (in the case of spirals) only and exclusively by a physician experienced in the field.
Side effects
The undesirable effects caused by the use of implantable hormonal sticks are the same as those described for oral contraceptives of the progestin type.
As for the spirals, however, they are generally well tolerated, but in some cases they can give rise to serious complications, such as infections and ectopic pregnancy.
Contraceptive Ring
The contraceptive ring, similarly to what happens for the spirals, must be inserted into the vagina, inside which it will then release the active ingredients (estrogen and progestin) contained therein. Generally, these active ingredients are "ethinyl estradiol and" etonogestrel (NuvaRing®).
However, a physician is not required for the insertion procedure of this device. Therefore, the ring can be safely inserted and removed by the patient herself.
The contraceptive mechanism of action and the side effects deriving from the use of the contraceptive ring are similar to those previously described for oral contraceptives in combination.
In any case, for more information, please refer to the dedicated articles "Contraceptive Ring" and "Contraceptive Ring: Advantages and Disadvantages".
Barrier Contraceptive Methods
Barrier - or mechanical - contraceptive methods are contraceptive devices that perform their action by preventing direct contact between the egg cell and the spermatozoa.
Among the different devices belonging to this category we remember the condom, the contraceptive diaphragm (to be used preferably in combination with spermicides), the cervical cap and the female condom.
This type of contraceptive will not be addressed in this article. Therefore, for more detailed information on this subject, please refer to the reading of the dedicated articles on this site: "Mechanical Contraceptives - Barrier Methods", "Condom - Condom", "Contraceptive Diaphragm", "Cervical Cap" and "Female Condom" .
Emergency contraceptives
The term "emergency contraception" refers to a method that is able to prevent the onset of pregnancies following unprotected sexual intercourse, or following the failure of a contraceptive method (such as, for example, rupture of the condom).
This type of contraceptive therapy can be based on a single contraceptive agent, as in the case of the so-called "five days later pill" based on ulipristal acetate (EllaOne®) and as in the case of the well-known "morning after pill" containing levonorgestrel ( Norlevo®); or it can be based on an estrogen-progestogen combination.
The most common side effects deriving from the use of this type of contraceptive are nausea and vomiting.
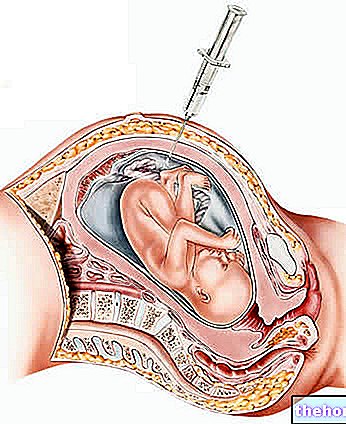
In the event that the patient cannot take hormonal contraceptives, then the doctor may decide to intervene by implanting a copper IUD within five days of unprotected intercourse or ovulation.













.jpg)











