Generality
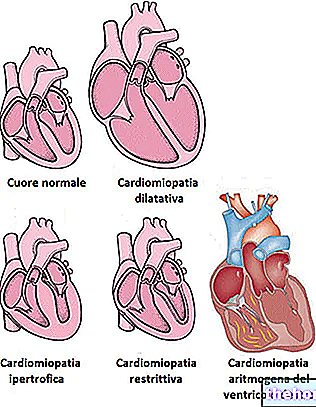
Antiarrhythmic drugs are medicines that are used in the treatment of cardiac arrhythmias.

The heart rhythm is normally controlled by a defined peacemaker site sino-atrial node it is made up of specialized cells that contract, generating action potentials.
The rate of cardiac contraction at rest should be included in a range that goes, approximately, from 60 to 100 beats per minute. If the sinus velocity is less than this range, we can speak of bradycardia; on the contrary, if the sinus speed is higher than the aforementioned values, then we speak of tachycardia. In any case, in these cases we always and in any case speak of cardiac arrhythmias, whether they are bradycardic or tachycardic.
The antiarrhythmic drugs currently used in therapy can be divided into various classes, according to the effect they exert on the action potential of the myocardial cells. These classes will be briefly described below.
However, to better understand the classification typology and the mechanism of action of antiarrhythmic drugs, it is necessary to make a small premise on what the aforementioned cardiac action potential is and how it is generated.
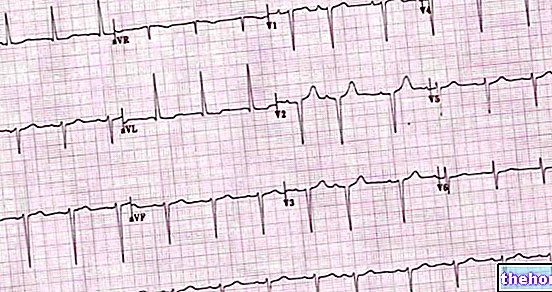
Cardiac action potential
As mentioned, the cells of the myocardium contract, generating an action potential, the course of which, under normal conditions, is absolutely predictable.
The aforementioned cardiac action potential can be divided into five phases:
- Phase 0 or phase of rapid depolarization: in this phase the permeability of the cell membrane for sodium ions increases, allowing the rapid entry of this cation into the cell and causing a rapid depolarization. When the heart cell is at rest, in fact, the internal membrane potential is more electronegative than the external one (this is defined as membrane potential at rest). When the impulse arrives and enters the zero phase, instead, there is a rapid inversion of the internal membrane potential, which becomes positive with respect to the outside.
- Phase 1: in phase 1 the permeability of the membrane to sodium ions is reduced and there is the entry of chlorine ions into the cell and the exit of potassium ions.
- Phase 2: phase 2, also called plateau phase, is characterized by a slow entry into the cell of calcium ions, counterbalanced by the release of potassium ions. This phase is called plateau precisely because there is little or no change in the potential. membrane.
- Phase 3: in this phase the entry speed of calcium ions slows down in conjunction with a continuous efflux of potassium ions. All this brings the membrane back to its initial resting potential.
- Phase 4: in this phase, finally, we witness the restoration of ionic concentrations inside and outside the cell, thanks to the action of the membrane Na + / K + ATPase pump.
Briefly summarizing, we can state that the action potential is generated by an initial entry of sodium ions into the heart cell, followed by the entry of calcium and, finally, by the exit of potassium which brings the action potential back to the condition rest.
Class I antiarrhythmics
Class I antiarrhythmics perform their action through the binding and consequent blocking of sodium channels.
These antiarrhythmics can in turn be divided into subclasses. Therefore, we can distinguish:
- Class IA antiarrhythmics: the active ingredients belonging to this class of antiarrhythmics block the sodium channel by inhibiting phase 0 of rapid depolarization, thus prolonging the action potential. This type of antiarrhythmics dissociates from sodium channels at a rapid rate. intermedia. This class includes active ingredients such as quinidine, disopyramide and procainamide.
- Class IB antiarrhythmics: antiarrhythmics belonging to this class always work by blocking sodium channels, but dissociate from them much faster than class IA antiarrhythmics and give rise to a short phase 3 of repolarization, thus also reducing the duration of the action potential. Thanks to their rapid onset of action, they are mainly used in emergencies.
Lidocaine (effective only if administered parenterally), tocainide, mexiletine and phenytoin belong to this class of antiarrhythmics. - Class IC antiarrhythmics: these antiarrhythmics have a low rate of dissociation from sodium channels and give rise to a very slow initial phase 0 depolarization.
Active ingredients such as flecainide, propafenone and moricizina belong to this category.
Side effects
Being a rather heterogeneous class, the side effects deriving from the use of class I antiarrhythmics can vary greatly, depending on both the type of active ingredient chosen and the route of administration (parenteral or, where possible, oral) and "intends to employ.
For example, the main side effects that can occur following the use of quinidine are gastrointestinal (abdominal pain, vomiting, diarrhea and anorexia), while the main undesirable effects deriving from the use of parenteral lidocaine consist of dizziness, delusions, paraesthesia and confusion.
Class II antiarrhythmics
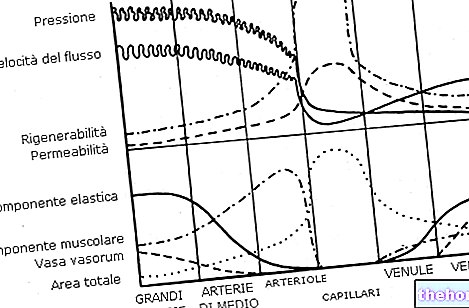
Class II antiarrhythmics are active ingredients with β-blocking action. More specifically, these active ingredients are able to block the β1 adrenergic receptors present in the heart. The stimulation of these receptors, in fact, causes an increase in the frequency, contractility and conduction speed of the impulse of the myocardial cells.
The blocking of this type of receptors, on the other hand, causes a blockage of the influx of calcium ions inside the cell, thus inducing a prolonged repolarization. This class of antiarrhythmic drugs includes active ingredients such as propranolol, sotalol, nadolol, "atenolol," acebutolol and pindolol.
Side effects
Also in this case the type of undesirable effects that may occur depends very much on the active ingredient used and on the sensitivity of each patient towards the drug.
In any case, the main side effects deriving from the intake of β-blocking antiarrhythmics are: dyspnoea, headache, dizziness, fatigue, bradycardia and Raynaud's syndrome.
Class III antiarrhythmics
Class III antiarrhythmics are active ingredients that exert their activity by inhibiting the repolarization of the membranes of heart cells. More specifically, these antiarrhythmics interfere with phase 3 of the action potential by blocking potassium channels.
Active ingredients such as ibutilide and amiodarone belong to this class of antiarrhythmic agents.
The main side effect deriving from the use of this type of antiarrhythmics is hypotension, including that of the orthostatic type.
Class IV antiarrhythmics
Class IV antiarrhythmics exert their activity by blocking calcium channels, thus giving rise to a slow repolarization phase of the cell membrane.
Among the various active ingredients belonging to this class of antiarrhythmics we mention verapamil and diltiazem.
The side effects that can arise following the intake of class IV antiarrhythmics consist essentially in hypotension, confusion, headache, peripheral edema, pulmonary edema and, in some cases, constipation.
Other antiarrhythmic drugs
There are other drugs with antiarrhythmic action that do not fall within the classification just made. This is, for example, the case of adenosine and digitalis glycosides.
Adenosine is a nucleoside that can be used - at the appropriate dosages and intravenously - in the treatment of paroxysmal supraventricular tachycardias. Adenosine exerts its action by acting directly on the atrioventricular node of the heart.
Among the digitalis glycosides, on the other hand, we remember digoxin, an active principle used above all in the treatment of atrial fibrillation and flutter. Digoxin exerts its antiarrhythmic activity by inhibiting the membrane Na + / K + ATPase pump, resulting in increased intracellular sodium levels.