Generality
Placental abruption occurs when the placenta is prematurely and unusually detached from the uterus. If severe, this event is life threatening to both mother and fetus. The exact cause is unknown, but the There are numerous risk factors involved.

Unfortunately, there is no treatment that can reattach the placenta. However, if action is taken promptly, it is possible to save the life of the fetus and the mother. Hemorrhage is answered with transfusions, even large ones, of blood.
The placenta
The placenta forms inside the uterus during pregnancy to nourish, protect and support the growth of the fetus. It is therefore a temporary or deciduous organ.
The placenta has a dual origin: maternal and fetal. The maternal component derives from the endometrium of the uterus; the fetal component corresponds to the chorionic villi (or chorionic villi). The chorionic villi are branched extensions of the placenta, which sink into the uterus (inside the "lacunae"), to withdraw nutrients and oxygen from the mother's blood vessels. At this point, nourishment and oxygen convey towards the umbilical cord and, from there, reach the fetus.
THE DIMENSIONS OF THE PLACENTA
At the end of pregnancy, the placenta takes on the following characteristics:
- It is blue-red in color and discoid in shape
- The diameter measures between 15 and 22 centimeters
- The thickness varies between 2 and 4 centimeters
- Weighs 500-600 grams (15% of the baby's weight)
THE MAIN FUNCTIONS OF THE PLACENTA
The placenta is essential for the survival and growth of the fetus. In fact, it is a multifunctional organ: it acts as a lung, kidney, digestive system, immune system and protective barrier.
- From the lung, because it supplies oxygen to the fetus and discharges carbon dioxide.
- From kidney, because it regulates the body fluids of the fetus.
- From the digestive system, because it supplies the fetus with nutrients, such as glucose, triglycerides, proteins, water, minerals and vitamins.
- From the immune system, because maternal antibodies reach the fetus through it, for defense against pathogens.
- As a protective barrier, because it blocks toxic substances for the fetus.
What is placental abruption?
Placental abruption (or placental abruption) is the premature separation of the placenta from the inner wall of the uterus.

Along with placenta previa, placental abruption is a major cause of bleeding antepartum, which is, in turn, one of the most important reasons for maternal and fetal death.
N.B: it is considered hemorrhage antepartum any vaginal blood loss, occurring from the 24th week of gestation.
SEVERITY € OF POSTING
Based on the surface of the placenta, which detaches from the uterus, we speak of:
- Mild placental abruption. Characteristics: the surface of the placenta detached from the uterus is less than 1/4.
- Moderate placental abruption. Characteristics: the detached placenta surface varies from 1/4 to 2/3.
- Severe placental abruption. Characteristics: the surface of the detached placenta is more than 2/3.
Clearly, the greater the detached surface, the greater the gravity of the situation.
Furthermore, another factor affects the severity of placental abruption: the week of gestation in which the episode occurs. In fact, the more advanced the pregnancy, the more serious the consequences can be on the mother and the fetus.
WHEN DOES IT HAPPEN?
Placental abruption occurs most frequently in the last 12 weeks prior to delivery.
EPIDEMIOLOGY
One in 100 pregnancies is characterized by placental abruption. The latter causes about 15% of perinatal deaths and about 30% of hemorrhages antepartum.
The death of the mother, on the other hand, again due to a placental abruption, is a fairly rare event.
N.B: the perinatal period is the one that goes from the 27th week of gestation to the first 28 days of life of the newborn.
Causes
The precise cause of placental abruption is unknown; however, it has been found that certain circumstances favor its onset. Taken individually, these risk factors may not be enough to detach the placenta from the uterus; conversely, their concomitance is decisive.
But what are these risk factors?
RISK FACTORS
The list includes several situations, such as:
- Abdominal trauma.
Classic traumas are those reported after a car accident or a fall. - Multiple pregnancies.
The delivery of the first child can alter the anatomy of the uterus, to the point of causing separation of the placenta before the birth of the other fetuses. - Age of the mother.
Over 40 years old. - Alteration of blood clotting.
These are disorders that change the blood's ability to clot. - Premature rupture of the amniotic sac.
The rupture of the membrane, which surrounds the amniotic sac, causes the amniotic fluid to leak out. This event makes it easier for the placenta to separate. - Hypertension.
It can be a chronic condition of the patient or resulting from pregnancy. - Previous placental abruption.
In these cases, there is a greater chance that the episode will repeat itself. - Smoking and drug abuse.
Placenta abruption is more common in women who smoke during pregnancy or who are addicted to cocaine. - Intrauterine infections.
They are due to pathogens originating from the vaginal cavity.
Other possible risk factors: multiparity and short cord.
Symptoms, signs and complications
Symptoms and signs that characterize placental abruption are:
In the pregnant woman
- Vaginal bleeding (haemorrhage ante partum)
- Abdominal pain
- Lower back pain
- Rapid contractions of the uterus (tetanus-like contractions)
- Shock
- Fragility of the uterus
In the fetus
- Oxygen deficiency (hypoxia)
- Abnormal heart beat (lower heart rate)
- Fetal distress
For most of these symptoms, there is a direct correlation between their severity and the severity of the placental abruption. The only symptom, which does not always follow this trend, is bleeding.
The details regarding the symptoms will be covered below.
THE BLOODING
Blood loss, or bleeding antepartum, is perhaps the most important symptom of placental abruption. As has been anticipated and differently from what one might think, the amount of blood lost externally by the mother is not always correlated with the severity of the detachment. On the contrary, the opposite occurs many times.
In fact, it is easier for the bleeding to remain almost entirely confined to the inside of the uterus, if the detachment is moderate-severe (hidden bleeding); and, on the other hand, it is more probable to observe a conspicuous bleeding towards the outside, if the detachment is slight (external bleeding). The explanation for this behavior is not known.

In light of this, minimal vaginal blood loss should never be underestimated, as it may require urgent intervention if it is due to a severe placental abruption. In these situations, fortunately, the strong abdominal pain felt by the pregnant woman has a fundamental significance and leaves little doubt.
Amount and frequency of bleeding
In quantitative terms, the blood lost (both due to external haemorrhage and hidden haemorrhage) is less than 1000 ml, in less severe cases; while, it is higher than 1000-1500 ml, in the most severe cases.
Finally, the percentages of frequency: 80% of cases of placental abruption present with external haemorrhage, while the remaining 20% is characterized by hidden haemorrhage.
CONSEQUENCES OF BLOODING
Blood loss affects the pregnant woman and the fetus.
To the damage of the pregnant woman, it determines a particular condition, called hemorrhagic or hypovolemic shock, which can also lead to death (in particular, in cases of an "extensive separation of the placenta).
To the damage of the fetus, on the other hand, it causes hypoxia, that is a general state of lack of oxygen, and fetal distress. Fetal distress is a vague term, which identifies a series of different disorders, including cardiac anomalies, reduced intrauterine growth and oligohydramnios. .
What is oligohydramnios?
The term oligohydramnios identifies a scarce presence of amniotic fluid in the amniotic sac. This condition does not usually affect pregnancy, but, in some unfortunate cases, it can have negative effects. A classic example is the reduction of space for fetal growth, which manifests itself, at birth, with physical malformations (valgus).
ACHE
The intensity of the painful sensation depends on the severity of the placental abruption. This means that the mild forms of placental abruption are characterized by weak pain, while the more severe ones present with very acute pain.
The site of pain is in the abdominal and lumbar level; the onset, on the other hand, can be sudden or gradual.
UTERINE CONTRACTIONS
Uterine contractions must arouse suspicion when more than one occurs every three minutes.
Severe placental abruptions are characterized by high-frequency uterine contractions. Therefore, as with pain, the latter become an evaluation parameter, to rely on, if there is no blood loss to the outside.
COMPLICATIONS
Complications, which arise from a detachment of the placenta, endanger the life of the pregnant woman and the fetus.
As far as the mother is concerned, coagulation disorders (DIC, disseminated intravascular coagulation), renal (or other organ failure) and the need for a hysterectomy (removal of the uterus) may be added to the haemorrhagic shock, which has already been discussed.
As for the fetus, however, in addition to hypoxia and fetal distress, premature birth or intrauterine death can occur.
WHEN TO SEEK A DOCTOR?
A pregnant woman should seek immediate medical attention or medical assistance when:
- He experiences abdominal and lower back pain
- Experience rapid uterine contractions
- She is prone to vaginal bleeding
Diagnosis
The diagnosis of a placental abruption is based on a physical examination, at your gynecologist, who evaluates the presence of the symptoms and signs described above.
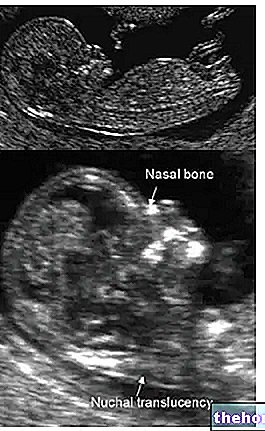
It is also possible to perform an "ultrasound", but its outcome is not always reliable. In fact, even if there is an ongoing placental abruption, the ultrasound images may show no anomalies. Given the danger and urgency of the situation, it is not It is possible to stick to an examination, in this case, not very exhaustive.
Therapy
Unfortunately, it is not possible to reattach the placenta to the uterus. However, there are some therapeutic countermeasures, which, in severe cases, save the life of the mother and fetus.
In general, in the presence of a placental abruption, the planned therapy consists of:
- A blood transfusion for the mother
- An early delivery
The urgency of these interventions depends on the gravity of the situation.
BLOOD TRANSFUSION
The transfusion serves to restore the volume of blood lost by the mother. The quantities transfused depend on the severity of the placental abruption.
- If the detachment is slight, 1000ml of blood is sufficient.
- If the detachment is moderate, 1500 ml of blood is needed.
- If the detachment is severe, 2500ml of blood is also needed, the first 500ml of which must be transfused very quickly.
When transfusion is performed, venous pressure should be measured at regular intervals. This is due to the fact that the injection of blood could raise blood pressure, with even dire consequences, such as pulmonary edema.
BIRTH: WHEN AND HOW TO INTERVENE?
Opting for an early birth, or not, depends on several factors, such as:
- Week of pregnancy
- Fetal distress
- Severity of the posting and state of health of the mother
If the fetus is still immature (before the 34th week of pregnancy) and does not show fetal distress, only a hospitalization of the pregnant woman is used, to closely follow the evolution of the situation and to restore the volume of blood lost. In these conditions, premature birth is almost never necessary; it becomes so when the conditions of the fetus or mother worsen.
If the pregnancy is at term (it is considered as such after the 34th week) and the placental abruption is minimal, the patient is hospitalized, as a precaution, while awaiting delivery; childbirth, which can be vaginal.
However, this situation changes if the placental abruption worsens or is already severe. In such situations, action must be taken immediately, by performing a caesarean section.
Finally, when the abruption of the placenta is so severe as to cause intrauterine death, vaginal birth is used to extract the fetus.
Prognosis and prevention
The prognosis of a placental abruption varies from patient to patient, based on several factors.
The first factor is certainly the severity of the detachment itself: mild forms require simple monitoring and a moderate blood transfusion; the severe forms, on the other hand, require large quantities of blood and an immediate delivery with an uncertain outcome.
The second factor concerns the quality of the care received by the mother. If the diagnosis is early and the medical treatment promptly (immediate transfusion, correct delivery, etc.), the prognosis tends to be positive, at least for the mother. Otherwise, the mother and fetus are life threatening.
According to some statistical studies, carried out in Finland between 1972 and 2005, the frequency of maternal death (i.e. of the mother) is one case for every 2500 women with placental abruption.
IS IT POSSIBLE TO HAVE OTHER PREGNANCIES?
The advice given to a woman intending to have another pregnancy, after a first one characterized by a detachment of the placenta, is to contact her gynecologist. The latter, having assessed the risks of a second conception, will tell you how to behave .
PREVENTION
Adopting a healthy lifestyle (not smoking, not using drugs, keeping blood pressure under control, etc.) helps prevent placental abruption.







.jpg)


















