Nuchal translucency, in acronym NT, is a screening test that assesses the risk of chromosomal abnormalities during the early stages of fetal life.
Statistically speaking, the interpretation of the results of nuchal translucency allows to identify 75-80% of fetuses affected by Down syndrome, with a false positive rate of 5-8%.

In addition to indicating an increased risk of trisomy 21 and other rarer chromosomal diseases (such as trisomy 18), nuchal translucency allows us to quantify the probability that the fetus is a carrier of certain skeletal and cardiac malformations.
When is it done?
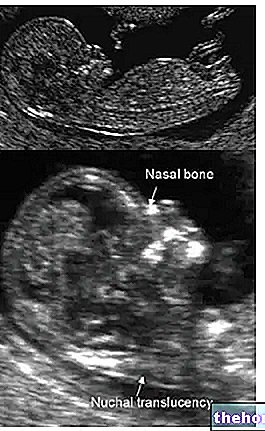
Nuchal translucency is performed between the 11th and 14th week of pregnancy, subjecting the pregnant woman's uterus to a series of sound waves that cannot be perceived by the human ear (ultrasound). These waves, absolutely harmless for both mother and fetus, are variously reflected by the tissues in relation to their density, then picked up by the same probe that generated them, converted into an electrical signal and processed by a computer to provide images of the tissues examined.
In the posterior region of the fetal neck there is an "area that does not reflect ultrasound, therefore anechoic and translucent; in this area we find a small physiological accumulation of fluid between the skin and the underlying paravertebral tissues. The collection of this fluid begins to appear around the 10th week of pregnancy and increases in thickness in the following weeks, and then decreases until it disappears after the 14th week.
Nuchal translucency: clinical significance
Scholars have noted that the excessive thickness of this translucent area (called nuchal fold) is attributable to an increased risk of Down's Syndrome or other chromosomal pathologies.
In general, the greater the thickness of the nuchal translucency, the greater the risk that the fetus is affected by chromosomal abnormalities (especially Down syndrome and less frequently by trisomy 13 or 18). Despite this, the increase in nuchal translucency is not always related to pathologies, but can be a momentary event; moreover, when it has pathological significance it can also be present in the absence of chromosomal defects, for example due to heart disease, metabolic alterations with hypoprotidemia , congenital or acquired anemia (infections), skeletal dysplasias, etc.
When it comes to nuchal translucency, it is important to remember that we are always and in any case talking about a screening test, and not an actual diagnostic test. The result of the examination, therefore, it does not tell us if the fetus is healthy or sick, but only the probabilities that it is. In other words, negativity reduces the risk but does not eliminate it, while positivity does NOT necessarily imply that the fetus is affected by the disease; rather, it requires further diagnostic tests, which will be carried out through the chromosomal examination on fetal cells after CVS or amniocentesis; these investigations, in general, are not performed directly as a first examination, because they are burdened by a very small but not negligible risk of abortion (0 , 5-1%).
Being a screening method, the "outcome of the examination" does not speak of positivity or negativity, but - thanks to the "help of a software developed by the Fetal Medicine Foundation (London) and the evaluation of other parameters (maternal age, weight, smoking) etc.) - expresses the risk in statistical percentage terms (for example 1 possible pathological case out of 1000 or one possible pathological case out of 100). If the study shows a positive risk profile, therefore, the report must not be confused with the ability of the test to identify fetuses affected by Down syndrome. Rather, it means that among all those cases for which the "examination reports" attention, there is a certain risk that requires further investigations ", also includes a certain percentage of fetuses actually affected by Down syndrome (in this case 75-80%) . At the subsequent amniocentic or villus examination, therefore, the vast majority of fetuses will be confirmed free of any chromosomal anomaly; this is because pregnant women with a risk profile equal to or greater than 1: 250 (one or more probabilities on 250 that the fetus is sick).
To improve the reliability of nuchal translucency as an early screening method for Down syndrome, the examination is now integrated with the so-called duotest, which consists in the simultaneous blood assay of chorionic gonadotropin (beta - β-hCG subunit) and PAPP- A (pregnancy-associated plasma protein).
An increase in β-hCG and a decrease in PAPP-A in the maternal venous blood are considered to indicate an increased risk of Down syndrome.
The concentrations of these two substances (PAPP-a and B-hCG) - multiplied by the intrinsic risk dependent on maternal age, and integrated with the ultrasound data of nuchal translucency - allow to recognize up to 90% of Down Syndrome cases. , with a percentage of false positives of 5%. Although these are respectable percentages, when the estimated risk is substantial, it is always and in any case suggested to undergo further invasive diagnostic tests. The fetal cytogenetic investigation, performed by means of CVS or amniocentesis , will therefore be able to exclude (as happens in most cases) or definitively confirm Down Syndrome, Trisomy 18 and other chromosomal anomalies.
The examination of the nuchal translucency can also be associated with the ultrasound examination of the nasal bone. Examining the profile of the fetus during the ultrasound, between the 11th and 14th week, in fact, has important implications in screening, since in this period about the 60-70% of Down syndrome fetuses do not show visible nasal bone.
A high nuchal translucency, even when the combined test (ultrasound + bi-test) is negative, can be associated with an increased risk of fetal structural anomaly (in particular, as already mentioned, affecting the heart). In this case, a 2nd level ultrasound is recommended to be performed at 16 and / or 20-22 weeks of gestation, with particular reference to the study of the heart.
PLEASE NOTE: The integration of the duotest with the nuchal translucency is called a combined test.
How is the nuchal translucency exam performed? How long does it last? Is it painful?
Sometimes the exam may last more than 30-45 minutes, due to the need to take multiple measurements with the fetus in well-established positions. For the same reason, the patient may be asked to cough or change positions, in order to determine the displacement of the fetus for a correct scan. The examination is sometimes hindered by particular conditions, such as maternal obesity or bulky fibroids of the anterior wall of the uterus.
It is essential that the detection of nuchal translucency is carried out by expert and qualified operators, so that the subsequent risk analysis can be standardized, precise and reliable.
Ultrasound measurement of the nuchal translucency it can be performed transabdominally or transvaginally; in the latter case, the examination allows to obtain a better resolution of the image and a correct scan, but it can also cause some discomfort to the pregnant woman.













.jpg)











