Colonoscopy is a diagnostic procedure aimed at direct vision of the internal walls of the large intestine (in particular of the colon).
Execution
During the examination a small flexible probe called colonoscope is used, equipped at the apex with a camera and light source.
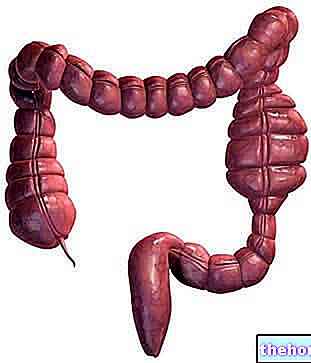
This probe, specially lubricated, is inserted into the anus and made to go up slowly in the rectum and in the other sections of the large intestine, meeting in the order sigma, descending colon, transverse colon, ascending and blind colon (see figure below); reached the last part of the small intestine, called ileum, the colonoscope is withdrawn with equal delicacy.

Thanks to the camera, during the colonoscopy the doctor can appreciate the state of health of the colon by observing the images transmitted by the instrument to the special screen.
In order to ensure a better visualization of the colonic mucosa, during colonoscopy it is necessary to relax the intestinal walls, which is obtained by insufflating carbon dioxide through the colonoscope. This can cause some discomfort to the patient.

During the entire operation, the patient remains lying on his left side, but the doctor can be asked to perform small movements.
Painkillers and tranquilizers are usually given before starting the colonoscopy, to make the examination more comfortable and lessen the unpleasant sensations.
Overall, the investigation takes about 30-40 minutes.
What is it for?
The main application of colonoscopy lies in the investigation of the state of health of the colonic mucosa, in order to identify any lesions, ulcerations, occlusions, tumors or polyps.
Interventional colonoscopy
In addition to acting as a video camera and insufflating air, the colonoscope can - if necessary - clean the walls of the colon with water, aspirate the intestinal contents or act as a vehicle for surgical instruments with which to perform tissue sampling or remove polyps.
Colonoscopy is therefore not exclusively for diagnostic purposes, but can also be used to perform biopsies and therapeutic interventions. In this case we speak of interventional colonoscopy.
Insights on Colonoscopy
Indications
Colonoscopy essentially recognizes two major fields of application: colon cancer screening and the search for diagnostic elements in the presence of intestinal signs and symptoms.
COLONSCOPY AND COLON CANCER
The examination can be performed as a first or second level investigation for colon cancer screening. For the population without major risk factors beyond age, the guidelines recommend performing a colonoscopy or sigmoidoscopy between 58 and 60 years, to be repeated every decade. The two examinations are based on the same methodological principles, with the difference that sigmoidoscopy is limited to the endoscopic study of the last section of the colon; its main disadvantage is that just under half of adenomatous polyps and tumors are formed in upper traits, while on the other hand it exhibits the important advantage of being less invasive than and exposing the patient to a lower degree of risk. Colonoscopy, on the other hand, despite being considered the "gold standard" for the screening of colon cancer, requires more tedious preparation, a longer run time and has a higher risk of negative side effects (such as intestinal perforation and bleeding), which can occur in 2-3 cases out of 1000 tests. For this reason, in people at medium-low risk, colonoscopy is mainly used as a second level investigation after the detection of occult blood in the stool or polyps by sigmoidoscopy.
In the presence of other risk factors, such as colon polyposis or familiarity with this and other forms of cancer, the doctor may recommend performing a colonoscopy as a first-level investigation starting from 40/50 years of age every five or ten years.
COLONSCOPY AND DIAGNOSIS OF INTESTINAL DISEASES
In addition to colorectal cancer screening, colonoscopy is typically used to investigate the origins of symptoms such as abdominal pain, rectal bleeding, chronic constipation or diarrhea, frequent changes in the alvo (periods of constipation alternating with diarrheal episodes), anemia iron deficiency of unknown origin, tenesmus (sensation of incomplete evacuation of faeces), emission of ribbon-like excrements and abundant presence of mucus in the faeces Many of these symptoms are also attributable to cancerous forms of colorectal cancer.
Is colonoscopy painful?
Although many people are reluctant to the idea, especially because of the embarrassment associated with the particular diagnostic procedure, colonoscopy is usually well tolerated. Even if the examination is undoubtedly very annoying, the action of the painkiller and the tranquilizer, in general, is able to greatly attenuate the unpleasant sensations.When the colonoscope is moved or used to blow air, the patient may experience mild abdominal cramps or an urge to evacuate; any biopsies are usually painless. The "annoyance" of the examination is however largely influenced by the "skill of the operator" and the anatomy of the colon.
All these problems are overcome through an alternative technique which is only slightly less effective than the standard procedure. We are talking about the virtual colonoscopy, which unlike the previous one does not require the insertion of the probe and the use of sedatives to calm the pain, since it uses a special radiological equipment kept outside the patient. Despite this, virtual colonoscopy has the major limitation of not being able to intervene with biopsies or excisions of any polyps found.
Risks and Side Effects
Colonoscopy is a low-risk diagnostic test; Major complications statistically occur in about 3 in 1,000 cases, and can be caused by:
- sedatives used during the examination,
- accidental perforation of the colon
- any bleeding following removal of polyps or other abnormal tissues.
Among these, the most serious complication (<1 in 2,000 cases) is colonic perforation, which requires immediate major surgery.
Any blood loss can instead be stopped by cauterization already during the colonoscopy, which must be repeated for this purpose if the bleeding occurs without stopping spontaneously in the days following the first examination.
The other complications relate to the effect of sedative drugs on people at risk, such as heart patients.
Contraindications
Colonoscopy is not recommended in case of acute diverticulitis, toxic megacolon and in recovery from surgery in this part of the intestine, due to the greater susceptibility to the risk of intestinal perforation.
After the Colonoscopy
At the end of the colonoscopy, 30 to 120 minutes of hospitalization may be required, so that the effect of the sedatives used is attenuated; also for this reason it is generally recommended to go to the appointment in the company of an assistant and rest for the rest. of the day (the drugs used could cause drowsiness and fatigue; driving a vehicle is therefore strongly discouraged, as well as involvement in other activities that require "careful vigilance).
Flatulence and bloating are quite common problems at the end of the exam, due to the air blown in during the colonoscopy. As for nutrition, during the rest of the day preference will be given to light and easily digestible foods.
Even if - especially in patients undergoing biopsy or polypectomy - a slight loss of blood from the anus in conjunction with the first defecation following colonoscopy is quite normal, repeated blood loss justifies immediate medical consultation. The same applies if abdominal pain or high fever should appear in the following days.
Other articles on "Colonoscopy"
- Preparation for Colonoscopy
- Colonoscopy Diet
- Prepare for Colonoscopy with Herbs
- Diet after colonoscopy
- Virtual Colonoscopy
Colonoscopy - Video: How and When to Perform It
Problems with playing the video? Reload the video from youtube.
- Go to the Video Page
- Go to Wellness Destination
- Watch the video on youtube