An "intestinal ischemia may be caused by the occlusion of an artery responsible for carrying oxygenated blood to the intestine, or by the occlusion of a vein intended to collect the deoxygenated blood exiting the intestine." If the cause is the "occlusion of an" artery, the intestinal ischemia compromises the supply of oxygen to the intestine, so much so that it could even cause death by necrosis; if the cause is instead the "occlusion of a vein, the" intestinal ischemia alters the blood circulation out of the intestine, inducing a reflux of blood which leads to bleeding and edema.
Intestinal ischemia is a serious medical condition that requires prompt and appropriate treatment.
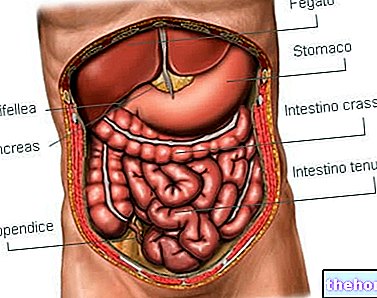
As it is known, the health of the tissues and organs of the human body depends on a correct blood circulation, both in and out; therefore, the presence of intestinal ischemia represents a real suffering for the intestine, which it jeopardizes its functioning and, in some situations, even risks its survival.
having relations with the intestine. In most cases, the blood vessel involved is an artery responsible for supplying the intestinal organ with oxygenated blood; more rarely, it is a vein belonging to the vascular system that has the task of draining the blood poor in oxygen from the intestine and lead it to the portal vein.
The first situation - occlusion of an "artery - is an example of arterial intestinal ischemia, while the second situation - occlusion of a vein - is an example of venous intestinal ischemia.
Arterial Intestinal Ischemia: Consequences, Types and Causes
Arterial intestinal ischemia involves a reduction in the supply of oxygenated blood to the intestine. The oxygen supplied by the blood is essential for the correct functioning and survival of any human tissue and organ; therefore, its deficiency in the intestine puts the intestine in difficulty, from a functional point of view, and, in the most serious situations (prolonged deficiency), can cause death by necrosis (intestinal infarction).
There are 2 types of arterial intestinal ischemia: the so-called ischemic colitis, whose target is the large intestine (colon in particular), and the so-called mesenteric ischemia, whose target is the small intestine.
ISCHEMIC COLITIS
Ischemic colitis is by far the most common form of intestinal ischemia in the general population. Although it can affect individuals of all ages, this condition most frequently affects people aged 60 and over (therefore those who are approaching advanced age).

Generally, ischemic colitis is due to a thromboembolic phenomenon related to atherosclerosis; however, it should be noted that, among the causes of this common type of intestinal ischemia, there are also:
- The intestinal volvulus;
- The abrupt and sudden drop in blood pressure (hypotension), resulting from a state of heart failure, trauma, shock or surgery that resulted in complications;
- The so-called intestinal adhesions;
- Advanced-stage colon cancer;
- Vasculitis affecting the arteries that supply the large intestine, inflammatory diseases such as systemic lupus erythematosus (SLE) and sickle cell anemia;
- The use of certain drugs, such as drugs with a vasoconstrictor effect, drugs for the treatment of heart disease, drugs for the treatment of migraine and hormonal drugs (eg estrogens);
- The use of drugs such as cocaine, amphetamines and methamphetamines;
- Excessive physical exertion, resulting from, for example, a long-distance run.
MESENTERIC ISCHEMIA
Mesenteric ischemia can be acute (acute mesenteric ischemia) or chronic (chronic mesenteric ischemia).
To distinguish "acute mesenteric ischemia from" chronic mesenteric ischemia is the way in which the phenomenon of reduction of the supply of oxygenated blood to the small intestine takes place: while in the first (acute) situation the aforementioned phenomenon is sudden (ie it occurs in a short period of time), in the second (chronic) situation the same phenomenon is gradual (ie it is the result of a progressive process).

Acute mesenteric ischemia recognizes at least 3 different causes, which are:
- The occlusion of the superior mesenteric artery following the arrival in the latter of an abnormal blood clot (embolus), originating in the heart.
This circumstance is, by far, the most common cause of acute mesenteric ischemia. - The occlusion of the superior mesenteric artery triggered by the formation of a thrombus on the latter wall. Normally, the thrombus in question results from the lesion of an atheroma, that is the classic cholesterol deposit that narrows the arterial vessels suffering from atherosclerosis.
- The reduced blood flow along the superior mesenteric artery which can result from the sudden drop in blood pressure, induced by: severe shock, heart failure, kidney failure or the use of certain medications.
This particular subtype of intestinal ischemia is also called non-occlusive ischemia, as it does not depend on an occlusive phenomenon, but on an "alteration of blood circulation."
Chronic mesenteric ischemia, on the other hand, is correlated, in fact, to a single causal factor, which is the occlusion of the mesenteric artery due to the singular and slow process of expansion of an atheroma present in the aforementioned artery (therefore, the ischemia chronic mesentery depends on atherosclerosis).
Curiosity
In the medical field, chronic mesenteric ischemia is also known by the curious name of intestinal angina.
Venous Intestinal Ischemia: Consequences and Causes
In venous intestinal ischemia, the obstructive phenomenon prevents the blood from continuing along the venous path provided for him and this triggers the reflux (ie the return to the vessels of origin) of the same.
In other words, intestinal venous ischemia, resulting in an obstacle to blood circulation within the intestinal veins, causes blood to flow backwards.
The reflux of venous blood caused by intestinal venous ischemia is responsible, in the intestine, for bleeding and edema.
CAUSES OF VENOUS INTESTINAL ISCHEMIA
Venous intestinal ischemia is caused by occlusion exerted by an abnormal blood clot (embolus), affecting the mesenteric vein or one of its branches.
Such a clot can result from various conditions, including:
- An acute or chronic pancreatitis;
- Infection of an abdominal organ;
- A tumor affecting an abdominal organ;
- Bowel disease, such as ulcerative colitis, Crohn's disease or diverticulitis
- Strong trauma to the abdomen;
- Coagulation diseases that promote the coagulation process (hypercoagulation).
Being related to a thromboembolic phenomenon, intestinal venous ischemia is also known as mesenteric venous thrombosis.
the lower left quadrant, followed over the next 24 hours by the presence of red or brown blood in the stool.When it concerns the ascending colon (right colon), ischemic colitis causes severe and sudden abdominal pain in the right lower quadrant, with little or no blood in the stool.
Acute Mesenteric Ischemia: Symptoms
As a rule, acute mesenteric ischemia is responsible for severe abdominal pain (the most intense pain occurs when the cause is an embolus), combined with disorders such as: abdominal distension, abdominal pain, nausea, vomiting, abnormal bowel movements and need urgent to defecate.

Chronic Mesenteric Ischemia: the Symptoms
Chronic mesenteric ischemia produces postprandial abdominal pain (ie after meals), with a dull character and accompanied by cramps.
As a rule, this pain begins 10-30 minutes after eating and reaches its peak of intensity after 2-3 hours.
Being responsible for post-prandial suffering, chronic mesenteric ischemia induces the patient to abstain from eating, which causes an involuntary decrease in body weight.
Venous Intestinal Ischemia: Symptoms
Venous intestinal ischemia is usually the cause of:
- Abdominal pain. This pain is less intense than the aching sensation that characterizes episodes of arterial intestinal ischemia, whether they are affecting the small intestine or the large intestine;
- Nausea and vomit;
- Diarrhea with or without blood in the stool.
Complications
In the absence of timely and adequate treatment or when it is very severe, intestinal ischemia can degenerate into complications such as:
- Death by necrosis of the intestinal tract involved in the ischemic phenomenon. Also known as intestinal infarction, this complication is possible when there is a complete blockage of blood circulation;
- Perforation of the intestine wall victim of the ischemic process. The perforation of the intestinal wall involves the leakage of the contents of the intestine, a phenomenon, the latter, which predisposes to the development of peritonitis (infection of the peritoneum);
- Formation of scars on the intestine, followed by the narrowing of the lumen of the latter. These scars result from the healing process triggered, sometimes, by the human organism, to cope with intestinal ischemia;
- Death of the patient.
When to see a doctor?
Especially in a subject at risk (e.g. an individual suffering from a coagulation disorder), the sudden appearance of an abdominal pain is always a valid reason to consult a doctor, or to go to the nearest hospital center, associated with impaired intestinal motility and disorders such as blood in stool, nausea, vomiting, abdominal cramps, abdominal distension and abdominal pain.
, blood tests, "observation from the inside of the intestinal tract by endoscopy, colonoscopy and / or sigmoidoscopy, diagnostic imaging with reference to the abdomen (CT, magnetic resonance and / or ultrasound)," peripheral angiography and " surgical exploration of the abdomen.with stenting (procedure that allows to eliminate an "arterial occlusion through the use of a catheter-a-balloon) or bypass (surgical operation for the creation of an alternative route to the passage of blood).
In the presence of damage to the intestine, it is essential to perform surgery to remove the damaged intestinal tract.
Did you know that ...
Some forms of ischemic colitis can heal spontaneously, that is, without resorting to particular treatments.
Acute Mesenteric Ischemia
- If the cause is an embolus, therapy for this type of intestinal ischemia includes anticoagulation, vasodilator therapy and, in the most severe cases, an embolectomy (to remove the embolus responsible for the obstruction).
- If the cause is a thrombus, the treatment mainly revolves around an angioplasty with stenting.
- Whether the cause is heart failure or kidney failure, therapy involves controlling these conditions.
- If the cause is the use of a certain drug, the cure consists in "stopping" the intake of the aforementioned medicine.
If there is damage to the intestine, acute mesenteric ischemia also requires surgery to remove the damaged intestinal tract.
Chronic Mesenteric Ischemia
The therapy for this form of intestinal ischemia can consist in the insertion of an arterial bypass or in the intervention of angioplasty combined with stenting.
Venous Intestinal Ischemia
In the absence of damage to the intestine, the therapy for this type of intestinal ischemia involves the intake of anticoagulants for 3-6 months, in order to dissolve the clot or blood clots that cause blood reflux.
If there is a bleeding disorder, anticoagulation therapy is for life.
In the presence of damage to the intestine, the treatment includes the same anticoagulant treatment mentioned above and, in addition, an operation to remove the damaged intestinal tract.