With still uncertain causes and very often asymptomatic, monoclonal gammopathy can evolve, in some rare cases, into very serious malignancies, such as multiple myeloma or lymphoma.
To detect monoclonal gammopathy, some blood tests are sufficient; nevertheless, many doctors prefer to investigate the situation with further tests.
As long as the condition remains asymptomatic, no treatment is provided.
In fact, the only medical indication is to periodically monitor the progress of the condition by means of appropriate blood tests.
Brief reminder of the bone marrow and its functions
The bone marrow is a soft tissue present in the internal cavity of some bones (femur, humerus, vertebrae, etc.). Its job is to produce blood cells, that is, red blood cells (or erythrocytes), white blood cells (or leukocytes) and platelets (or thrombocytes).
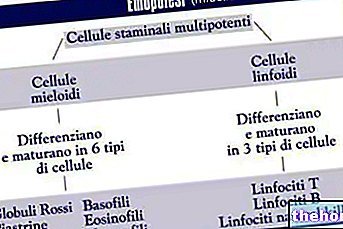
This process is called hematopoiesis (or hematopoiesis) and starts with particular cells, known as hematopoietic stem cells. The latter are real progenitor cells, capable of continually replicating and meeting different destinies, transforming themselves into:
- Red blood cells: carry oxygen to the tissues and organs of the body.
- White blood cells: they are part of the immune system and defend the body from pathogens and anything that can harm you.
- Platelets: are among the main actors of coagulation.

Figure: hematopoiesis starting from totipotent stem cells. Different types of stem cells derive from these, including hematopoietic ones. Hematopoietic stem cells have the gift of replicating continuously and of choosing whether to become red blood cells, white blood cells or platelets. : www.liceotorricelli.it
Please note: "emato" and "emo" mean "blood", while "poiesi" comes from the Greek verb "poieo" which means "to do" or "to produce".
; however, according to what emerges from numerous clinical cases, it can represent the prelude to various forms of cancer of the immune system or blood cells.
What is the immune system?
The immune system is the defensive barrier of an organism against threats coming from the external environment, such as viruses, bacteria or parasites, but also from the inside, such as for example the crazed tumor cells or the malfunctioning ones.
Taken as a whole, the immune system represents a complex integrated network that gathers within itself organs, cells and chemical mediators.
Located in various places in the body, the organs of the immune system (or immune organs) are: bone marrow, spleen, lymph nodes, tonsils and appendix.
Immune cells are the aforementioned white blood cells or leukocytes. There are numerous subpopulations of leukocytes: eosinophils, basophils / mast cells, neutrophils, monocytes / macrophages, lymphocytes / plasma cells, and dendritic cells.
Finally, immune chemical mediators are signaling molecules which, interacting with the various cells of the immune system, exchange information and regulate the level of defensive activity. In other words, they coordinate immune responses.
There are three different types of lymphocytes: B lymphocytes, T lymphocytes, and natural killer lymphocytes.
Plasma cells are B lymphocytes which, after contact with a certain class of antigens, have evolved and specialized in counteracting this class of antigens. Immunology books also refer to them as activated B lymphocytes.
The defensive action of plasma cells is based on the production of particular glycoproteins, known as immunoglobulins or antibodies. Being a highly specialized and selective defensive action, each plasma cell produces immunoglobulins all the same and all responsible for fighting only the antigen that activated the B lymphocyte in plasma cell.
Immunoglobulins have a conformation that is very reminiscent of the Greek letter gamma (γ): for this reason they are also called gamma globulins. Once produced by plasma cells, they do not personally destroy the antigen they have to fight, but they bind to it and make it visible and more susceptible to the action of other cells of the immune system (phagocytes and cytotoxic cells). In other words, antibodies act as signalers: they mark the foreign substance so that other immune cells can recognize and destroy it.
Why does Monoclonal Gammopathy arise?
Currently, doctors and researchers have not yet clarified precisely what exactly alters plasma cells and induces them to produce an abnormal protein.
Research has shown that the onset of monoclonal gammopathy is associated with some infections and some autoimmune diseases, such as rheumatoid arthritis.
Note: People with an autoimmune disease have an improperly acting immune system. In fact, through its countless cells, it attacks and damages healthy tissues and organs.
Epidemiology and Risk Factors
Monoclonal gammopathy is considered a rather rare condition; however, there is no more precise information relating to its exact diffusion in the general population.
Regarding risk factors, various studies have found that monoclonal gammopathy affects the most:
- The elderly, especially those over the age of 85. Older age appears to be one of the most important predisposing factors.
- People of color. Hence, it appears that ethnicity plays a certain role.
- Male subjects.
- Individuals with a family history of this disease. From this it was hypothesized that some cases of monoclonal gammopathy could be due to an "alteration of the genome, transmitted by inheritance.
When symptomatic, monoclonal gammopathy is distinguished by the presence of neurological problems, such as numbness and tingling in the hands and / or feet.
The cause of these neurological disorders is damage to the peripheral nerves, which is most likely caused by the paraprotein present in the blood. In fact, it seems that the monoclonal protein, when it flows through the blood vessels that nourish the peripheral nerves, favors the deterioration of the latter.
In medicine, the morbid condition that arises as a result of damage to the peripheral nerves is called peripheral neuropathy.
Complications
In some unfortunate circumstances, monoclonal gammopathy can develop into full-fledged diseases, including multiple myeloma, lymphomas, light chain amyloidosis or Waldenstrom's macroglobulinemia.
Furthermore, it should be noted that a worsening of monoclonal gammopathy can cause recurrent fractures and blood clots capable of affecting blood circulation (thromboembolism).
Typical symptoms of multiple myeloma
- Bone pains (particularly in the spine, pelvis, ribs, long bones and skull)
- Hypercalcemia. It causes excessive thirst, nausea, constipation, loss of appetite and mental confusion
- Kidney failure
- Anemia. It causes asthenia, generalized weakness and breathing difficulties
- Ease of infections
- Thrombocytopenia
- Hyperviscosity syndrome
- Neurological disorders including numbness, various nerve compression syndromes etc.
Multiple Myeloma and Lymphomas
Multiple myeloma is a specific malignant tumor of the immune system, characterized by such high levels of paraprotein, that problems arise in the kidney and beyond. In fact, those suffering from this serious neoplasm also develop: bone pain (affecting 70% of patients and representing the most common symptom), hypercalcemia, anemia, coagulation disorders (thrombocytopenia) and immune system deficiency (leukopenia).
Lymphomas, on the other hand, are malignant tumors that affect the lympho-glandular apparatus which constitutes the lymphatic system. B and T lymphocytes), prevents the tissues from accumulating excess fluids etc.
How to assess the risk of multiple myeloma or lymphoma in the case of monoclonal gammopathy?
According to doctors, to determine whether an individual with monoclonal gammopathy is more or less at risk of complications, the following parameters must be evaluated:
- The amount of paraprotein in the blood. Very high levels of M protein are very dangerous.
- The type of paraprotein present. Paraprotein does not always have the same characteristics in all patients. Some types of monoclonal protein appear to be more harmful than others.
- The amount of "free" light chains (also called Bence Jones proteins) in the blood. Immunoglobulins basically consist of two parts joined together: the light chains and the heavy chains. In an individual with monoclonal gammopathy, due to abnormal behavior by plasma cells, the light chains are not bound to the heavy chains and can be found in the blood. If they are particularly high, multiple myeloma is suspected.
When to see a doctor?
A person with previously asymptomatic monoclonal gammopathy should contact their doctor immediately if:
- He feels an extreme and unusual tiredness.
- Easily tends to trouble, even in the case of very simple activities.
- You suffer from constant pain in the bones and localized in specific points (for example in the back, hips, ribs or pelvis).
- Inexplicably he loses weight.
- It is particularly prone to infections. This is a clear sign of an immune problem linked to a white blood cell deficiency.
The use of further tests (urinalysis, other blood tests, X-rays, CT and bone marrow biopsy) is mainly used to assess the severity of the abnormality and the risk of complications.
Furthermore, a very accurate diagnostic procedure allows the identification of a multiple myeloma or a lymphoma.
Serum protein electrophoresis and immunoelectrophoresis
Serum protein electrophoresis allows to evaluate the quantitative levels of 5 serum proteins: albumin and α1, α2, β and γ globulins. In patients with monoclonal gammopathy, these 5 serum proteins present characteristic alterations, which a haematologist (a physician experienced in the diagnosis and treatment of blood diseases) is able to recognize.
Immunoelectrophoresis, on the other hand, allows the quantification of each type of immunoglobulin present in the blood. In people with monoclonal gammopathy, it allows the "identification of Bence Jones proteins, ie the" free "light chains.

Further blood tests
To investigate the situation, doctors use other blood chemistry tests, including:
- Complete blood count. It is used for an assessment (quantitative and not only) of red blood cells, white blood cells and platelets. It is useful in case of suspected lymphoma or multiple myeloma, because it allows to identify possible states of thrombocytopenia, neutropenia (decrease in the blood of neutrophilic leukocytes) etc.
- Creatinine measurement. Levels of creatinine in the blood are an index of renal activity. If they are elevated, it means that the kidneys are functioning poorly. Remember that multiple myeloma impairs kidney function, therefore, in these situations, creatinine is generally very high.
- Measurement of serum calcium. Finding large amounts of calcium in the blood could mean multiple myeloma.
Urinalysis
In people with monoclonal gammopathy and multiple myeloma, the urine contains Bence Jones proteins (in the latter case, the levels of "free" light chains are also very high).
Therefore, their examination serves as further confirmation of what has already been observed up to now with serum protein electrophoresis and immunoelectrophoresis.
X-ray
X-rays are useful in cases of suspected multiple myeloma, as this severe malignancy also involves the skeletal structure, resulting in bone abnormalities (also called rearrangements).
CT scan
CT (or computerized axial tomography) is a method that uses ionizing radiation to build a highly detailed, three-dimensional image of a given body compartment. It is completely painless, but the dose of X-rays to which patients are exposed is not it is negligible.
In the case of monoclonal gammopathy, it is practiced to evaluate the dimensional aspect of the lymph nodes, liver and spleen.
In some cases, to improve image quality, doctors may use a contrast fluid (gadolinium), which is injected into the blood and is not free from possible side effects.
Bone Marrow Biopsy
A biopsy consists of taking and histological analysis, in the laboratory, of a sample of cells from a certain tissue or organ.
On the occasion of a bone marrow biopsy, the collection of the cells to be analyzed takes place at the level of the iliac crests, by means of a special needle and after local anesthesia.
The subsequent laboratory analyzes are used to quantify the number of plasma cells (and paraprotein) present within the bone marrow.
At the end of the procedure, at the point where the needle is inserted, the patient may develop a small hematoma.
Caution: Doctors do a bone marrow biopsy only when they believe multiple myeloma is highly likely.
, corticosteroid drugs and hematopoietic stem cell transplantation. The latter, for reasons related to the availability of suitable donors, is more frequently of the autologous type than of the allogeneic type. However, it should be noted that allogeneic transplantation has a greater therapeutic potential.Patients over 65 years of age, on the other hand, are generally treated only with chemotherapy and corticosteroids (prednisone), as haematopoietic stem cell transplantation (whether autologous or allogeneic) is a contraindicated practice for health (NB: they may fail the procedure and develop serious complications).
Chemotherapy drugs expected in case of multiple myeloma
For patients under 65:
- Thalidomide
- Bortezomib
- Lenalidomide
For patients over 65:
- Melphalan
- Bortezomib
Other Treatments for Monoclonal Gammopathy
If patients suffer from recurrent bone fractures, a bisphosphonate-based treatment is provided to strengthen the bones (to be precise, they reduce bone resorption and increase bone mineral density).
Among the bisphosphonates, the most administered in case of monoclonal gammopathy are: zoledronic acid, alendronic acid (alendronate), risedronate and ibandronic acid.
Some advices
For people with monoclonal gammopathy, hematologists highly recommend:
- Find out about everything related to the condition that afflicts them. Knowing the possible symptoms, complications and surveillance diagnostics allows you to better control any change / evolution of monoclonal gammopathy.
On the contrary, neglecting the aforementioned aspects or knowing them only superficially could be very dangerous. - Adopt a healthy lifestyle. Eating fruit and vegetables, not smoking, exercising regularly and sleeping the right number of hours are behaviors that do not reduce the risk of complications, but make the onset of other diseases (comorbidities) less likely.
- Strictly adhere to the schedule of the check-ups. The mistake that some patients can make is to neglect the controls, because the latter, for some time, have given negative results.

-cosa-significa-quando-preoccuparsi.jpg)