What is Episclerite?
Episcleritis is a self-limiting inflammatory disease affecting the episcleral tissue.
The so-called "white of the eye", or more correctly sclera, is a fibrous membrane that covers a large part of the eyeball externally (approximately 5/6 of its surface).

The sclera is made up of two layers: the outermost one is called the episclera and is rich in connective tissue and blood vessels. The innermost layer is instead the sclera proper, formed by a loose connective tissue.
The sclera is externally covered by the conjunctiva; in the anterior part of the eyeball it borders the cornea, while posteriorly it lets the optic nerve pass.
Episcleritis typically presents with generalized or circumscribed redness of the eye, associated with mild eye pain in the absence of secretions and visual problems. Usually, the condition is idiopathic, so its cause remains unknown. In other cases, the condition is idiopathic. "Episcleritis can be associated with connective tissue or systemic diseases. Recurring episodes are common.
Therapy is symptomatic and includes the use of lubricating eye drops. Severe cases can be treated with topical corticosteroids or oral anti-inflammatory drugs (NSAIDs).
Causes
The episclera is a thin layer of tissue, which lies between the conjunctiva and the sclera. The redness of the eyes associated with episcleritis is due to congestion of the episcleral blood vessels, which extend radially.
Typically, there is no uveitis or thickening of the sclera. The disease is often idiopathic and an identifiable cause is confirmed in only one third of cases.
Episcleritis can be associated with an inflammatory, rheumatic or systemic condition such as:
- Systemic vasculitic diseases: polyarthritis nodosa and Wegener's granulomatosis;
- Connective tissue diseases: rheumatoid arthritis and systemic lupus erythematosus;
- Hyperuricemia and gout;
- Chronic inflammatory bowel diseases: ulcerative colitis and Crohn's disease;
- Rosacea, atopy, lymphoma and thyroid orbitopathy (pathology of the eye orbit of thyroid origin).
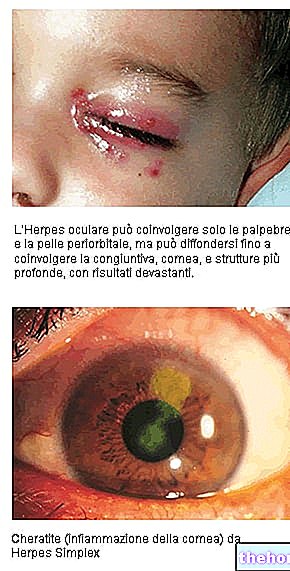
Infectious causes are less common; this is the case with: Herpes zoster, Herpes simplex, Lyme disease, syphilis, hepatitis B and brucellosis. Contact with chemicals or a foreign body can also cause episcleritis.
Rarely, the condition is caused by scleritis, a severe inflammation that occurs throughout the thickness of the sclera.
Episcleritis occurs most commonly in young adults, especially women. However, there are no specific risk factors for the disease.
Signs and symptoms
For further information: Episcleritis Symptoms
Symptoms of episcleritis include mild eye pain, globe hyperemia, irritation and tearing of the eyes. In addition, photophobia, eyelid edema, and conjunctival chemosis may be present. Ocular secretions are absent and vision is unaffected. The onset is acute or gradual, diffuse or localized.
There are two main types of episcleritis:
- Simple episcleritis: it is a recurrent but self-limiting inflammation which affects the episcleritis partially (simple sectorial episcleritis) or diffuse (simple diffuse episcleritis).
In the sectoral form, a bright red spot is present just below the bulbar conjunctiva. Simple episcleritis has an acute onset, lasts about 12 hours and then slowly resolves over the next 2-3 days (the total course lasts a maximum of two weeks). The episodes become progressively less frequent and, over the years, disappear completely. Simple episcleritis may be less painful than the nodular type.
- Nodular episcleritis: involves a "well-circumscribed area" of the episclera and is characterized by the presence of a small raised and translucent nodule in the inflamed area. In nodular episcleritis, the attacks are self-limiting but tend to last longer.
Episcleritis is distinguished from conjunctivitis by hyperemia localized to a limited area of the globe and by less profuse lacrimation. Also, the pain is less severe than in scleritis and photophobia is less than in uveitis. Episcleritis does not cause cells or blood to spill into the anterior chamber of the eye. Rarely, some cases may progress to scleritis.
Diagnosis
The diagnosis of episcleritis is clinical and is based on history and physical examination. Further investigation is needed for some patients in order to identify a possible underlying medical condition.
Episcleritis can be differentiated from scleritis by instillation of phenylephrine-based eye drops. This substance causes bleaching of the superficial and conjunctival episcleral vascular network, but leaves the underlying scleral blood vessels undisturbed. If a patient's eye redness improves after applying phenylephrine, the diagnosis of episcleritis can be confirmed.
Slit-lamp examination distinguishes nodular form from scleritis. Furthermore, it is important to note that the nodule is raised and freely movable relative to the underlying scleral tissue.
Treatment
Often, treatment is unnecessary, as episcleritis is a self-limiting condition. Most cases resolve within 7-10 days, but patients should be aware that episodes can recur in the same or the other eye. Nodular episcleritis is more aggressive and takes longer to heal (approximately 5-6 weeks).
Artificial tears can be used to relieve irritation. Severe or chronic / relapsing cases can be treated with corticosteroids and non-steroidal anti-inflammatory drugs for topical or oral use. These measures reduce inflammation and accelerate recovery. , but there are some risks associated with the use of steroid eye drops. The patient should therefore be closely monitored by the physician during therapy.
In general, episcleritis does not cause complications in the ocular structures; there may occasionally be corneal involvement (in the form of infiltration of inflammatory cells) or edema; in addition, recurrent attacks over a period of years can cause mild scleral thinning.



.jpg)