Trichotillomania is an obsessive-compulsive behavior disorder characterized by an irrepressible urge to pull and pull hair from the scalp.

Trichotillomania, if continued over time, causes the appearance of hairless patches at the level of the scalp or the areas of skin involved. The extreme need to pull one's hair is manifested as a response to a state of emotional tension, which does not find an outlet in an alternative way. Those suffering from trichotillomania are seized by a growing sense of tension and excitement, followed by a sense of relief at the completion of the pathological act. The subject, after the satisfaction phase, feels a strong sense of unease and guilt. Patients, in fact, are not able to stop this behavior, despite the repeated traction stresses causing evident and unpleasant hair loss. some people, trichotillomania can be mild and generally manageable. For others, the urge to pull the hair out is impossible to control and can be accompanied by significant personal and social discomfort.
Trichotillomania should not be confused with the habit of touching one's hair or with the normal habit of fiddling with it. Furthermore, the disorder is not related to baldness or alopecia. It is important to emphasize that hair loss does not occur spontaneously, but is the result of a pathologically self-induced and recurrent act. Although it may not seem particularly serious, trichotillomania can have a great impact Sometimes, this condition is self-limiting, but it is always advisable to seek immediate help from a doctor who can recommend the most suitable therapy.
Causes, incidence and risk factors
Trichotillomania is a type of obsessive-compulsive disorder. The causes at the origin of this behavior have not yet been clearly defined, but it is hypothesized that trichotillomania may derive from a combination of genetic, hormonal and environmental factors. Furthermore, the onset is strongly influenced by psychological reasons.
Trichotillomania occurs most commonly in children between 2-6 years of age and in adolescents, especially during the period that coincides with puberty. The most affected range is between 9 and 13 years. However, the condition can also manifest itself during adulthood, both in the case in which trichotillomania continues from "adolescence", and in the event that it arises from scratch following a triggering episode of a psychological nature, for example an event traumatic, medical intervention or for unresolved emotional difficulties, in the family or at work. In children and adolescents, trichotillomania can be present for limited periods of time, while if it occurs in adults it is usually a manifestation of malaise and emotional suffering of more concern. Trichotillomania affects about 4% of the population and affects mostly women. Most people with trichotillomania also have other disorders, including depression, anxiety or eating disorders. (onychophagy) and hair (ringworm) are obsessive-compulsive behaviors commonly associated with trichotillomania. For many patients, hair pulling is a way of coping with negative emotions or uncomfortable situations, such as stress, anxiety, tension, loneliness, fatigue, or frustration. Often, trichotillomania represents capable behavior. to give relief and satisfaction. The result can be a continuously repeated pathological act in order to maintain these positive feelings. In some cases, trichodynia, a disorder that manifests itself with persistent pain in the scalp, can be the triggering cause of trichotillomania.
How it manifests itself
The most obvious and unpleasant symptom of trichotillomania is alopecia, ie hair loss. In specific areas of the skin, patches are visible where there is no hair or hair, similar to what happens with some forms of alopecia areata. of the scalp in which the trichotillomaniac exerts the most manic behavior are the frontoparietal ones.
Trichotillomania signs and symptoms often include:
- Repeatedly twisting hair or hair, pulling it until it tears, resulting in noticeable hair and / or hair loss;
- Irregular and uneven appearance of the hair, associated with a regrowth of short and broken hair alongside other longer ones;
- Sparse or missing eyelashes or brows
- Hairless patches on the scalp or other areas of the body (trichotillomania rarely causes damage so extensive that it causes widespread growth failure throughout the head);
- Play with the uprooted hair (example: curling it around the fingers) or bite and eat it;
- Rub the torn hair on the face or lips.
Most people with trichotillomania:
- Try to deny or conceal the behavior;
- He experiences a growing sensation of tension before pulling his hair, followed by a sense of relief, pleasure or satisfaction once the tear has occurred;
- Feel embarrassed or ashamed of hair loss.
For some people, pulling their hair is an intentional and targeted behavior: they are fully aware of the fact that they are pulling them and can also elaborate particular rituals, choosing the right place and time to operate privately. Sometimes, the trichotillomaniac pauses to examine the extirpated hair, observing its shape, the size of the bulb, etc. or he arranges them in order on a surface on the basis of subjective criteria. Other people unconsciously pull out their hair while they are engaged in other activities. The same person can also manifest both behaviors, depending on the situation and mood. For example, the patient can manifest the disorder in specific contexts, during particularly frustrating and stressful periods, or in moments of boredom or inactivity. Certain positions or habits may prompt the need for hair pulling, such as resting the head on the hand.
Complications
- Damage to the hair. If continued over time, trichotillomania can cause irreversible damage, such as to make the hair bulbs atrophic. The functionality of the follicle, in some cases, cannot be restored.
- Damage to the skin. Constantly pulling on your hair can cause abrasions, dermatitis or other skin damage, including infections, localized to the scalp or to the specific area affected by the disorder.
- Hairballs or hair. The compulsive habit of eating torn hair (trichophagia) can lead to the formation in the gastrointestinal tract of a trichobezoar (or pilobezoar, if formed by hair), that is an indigestible mass, strongly intertwined and solid, which goes to localize itself in the stomach or in the "small intestine. Over a period of years, the bezoar can cause symptoms such as indigestion, stomach pain, food shortages, weight loss, vomiting and obstruction. The intestinal obstruction, resulting from the consumption of hair and / or hair, can extend to the duodenum or the ileum. This latter condition is called Rapunzel syndrome (the name derives from the tale of Rapunzel) and in extreme cases it can be lethal. The human gastrointestinal tract is unable to digest hair, so surgery may be required to remove the hair. bolus.
- Emotional stress. Many people with trichotillomania may experience a feeling of shame, humiliation and embarrassment due to their condition, and consequently suffer from depression and anxiety.
- Social issues. The embarrassment caused by hair loss can cause the patient to wear false eyelashes, wigs, hats, scarves or adopt a hairstyle to mask the hairless areas. People with trichotillomania can avoid intimacy situations for fear of their condition being discovered.
Diagnosis
Patients may not recognize the problem or actively try to hide it, at least until it manifests itself overtly by the evident abnormal loss of hair or hair in specific areas of the body. For this reason the diagnosis is not always immediate. patient does not admit to pulling his hair, it is certainly correct to consider other forms of ailments with symptoms similar to those of trichotillomania. Differential diagnosis includes evaluation for alopecia areata, tinea capitis, traction alopecia, discoid lupus erythematosus, folliculitis, and lax anagen syndrome.
The doctor will perform a thorough evaluation of the skin, hair and scalp. The exam aims to define the extent and frequency of the disturbance. A tissue sample (biopsy) may be pre-washed to look for other causes that may justify hair loss or the urge to pull hair. The biopsy reveals traumatized hair follicles with perifollicular hemorrhage, fragmented hair in the dermis and deformed hair shaft. In the case of trichotillomania, a lot of hair in the catagen phase will typically be seen. An alternative technique to biopsy, particularly for children, is to shave a portion of the affected area and observe the regrowth of normal hair. In case of trichotillomania, the "pull test" of the hair is negative (the procedure consists in gently pulling the hair by sliding it between the fingers, to evaluate how many are detached from the scalp).
According to the criteria of the DSM (Diagnostic and Statistical Manual of Mental Disorders) the presence of trichotillomania can be suspected when:
- Hair pulling is a recurring act, resulting in noticeable hair loss;
- The subject experiences a sense of increasing tension immediately before pulling out the hair or when trying to resist the impulse;
- While performing the act, a sense of pleasure, gratification or relief arises in the patient;
- The hair loss is not attributed to any "other medical or dermatological condition;
- The condition causes clinically significant distress.
Treatment
Trichotillomania must always be considered for the subjective meaning attributed by the individual patient. Frequently used treatments for trichotillomania include:
- Cognitive-behavioral therapy. Psychological therapy is the most widely used, as it is aimed at identifying the causal stimulus of trichotillomania. Cognitive-behavioral therapy is one of the most effective psychological techniques: it helps the patient to recognize the thoughts, feelings and triggers associated with the act of pulling one's hair. The goal of this therapy is to increase awareness of one's own behavior, to replace it with alternative and positive reactions. Furthermore, cognitive-behavioral therapy teaches to control the reactions to psychological impulses that force the patient to pull out hair and hair.
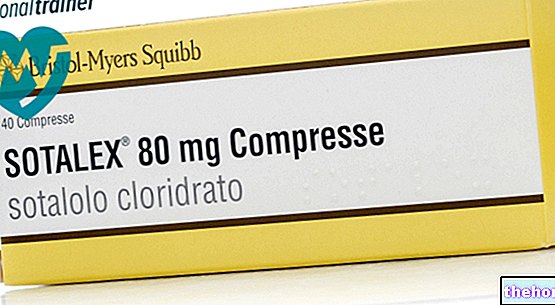
- Pharmacological therapy. Pharmacological therapy is used in the most severe cases, to decrease the anxiety, depression and obsessive-compulsive symptoms that accompany trichotillomania. If there is a sufficiently close correlation between the psychological distress that stimulates trichotillomania and the pathological act itself, by intervening with drug therapy the urge to pull hair should cease. Some selective serotonin re-uptake inhibitors (SSRIs), clomipramine (tricyclic antidepressant) and naltrexone (opioid receptor antagonist) have been shown to be effective in reducing some symptoms , but not all experts agree on the use of drugs for the treatment of trichotillomania.These should only be used in adult patients, after careful medical evaluation.
Most people who use targeted therapy can recover. Generally, if the disorder occurs in early childhood (before 6 years of age) it tends to be mild and disappear spontaneously without treatment. In adults, the onset of trichotillomania may be secondary to underlying psychiatric disorders and therefore may be more difficult to treat.
If the patient has overcome the compulsive behavior with an "adequate therapy, it is possible to resort to specific treatments to stimulate the still prolific follicles and make the fallen hair grow. Once removed from the harmful behavior, in fact, the hairs tend to grow back spontaneously. If the hair bulbs are seriously damaged, the last resort is surgical thickening with autotransplantation (trichological surgery). Early diagnosis is the best form of prevention, as it leads to an equally early and therefore effective treatment: resorting to therapy as soon as the first symptoms appear could help reduce any inconvenience to the person's life. There is no known way to prevent trichotillomania, although relieving stress can certainly limit the compulsive behavior underlying the problem.