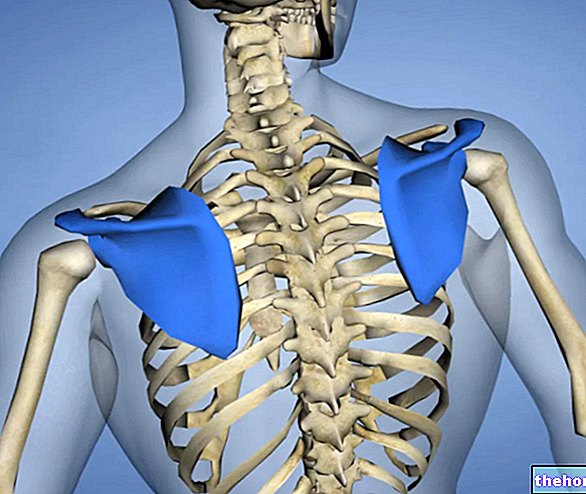
Epicondylitis is the generic term used to refer to a painful syndrome affecting the elbow area.
Due to the high incidence in tennis, epicondylitis is also nicknamed "tennis elbow".
![]()
It is caused by functional overload, or by an excessive and continued use of the joint. There is an individual predisposition but, as a result of incorrect attitudes, anyone could get sick with epicondylitis.
The sports most involved are: tennis, base ball, golf, fencing, badminton, squash, javelin or discus throwing, etc.
The most interested jobs are: plumber, bricklayer, gardener, carpenter, butcher, cook, carpenter, tailor, painter, etc.
Other activities affected are: playing, gardening (pruning plants) etc.
Epicondylitis mainly affects an age group between 30 and 50 years.
Initially symptomatic only during the movement of inflamed tendons, if severe the epicondylitis can worsen to the point of causing a painful picture even at rest.
The published material is intended to allow quick access to advice, suggestions and general remedies that doctors and textbooks usually dispense for the treatment of Epicondylitis; these indications must in no way replace the opinion of the treating physician or other healthcare specialists in the field who are treating the patient.
What to do
- Prevention is always the most effective means of reducing the possibility of injury (see under Prevention).
- Recognition of the disorder: when it comes to tendon compromises it is absolutely necessary to intervene promptly as they are difficult to heal. The symptoms are:
- Mild but worsening pain on the outside of the elbow.
- Swelling and pain when resting.
- Weakness in hand grip strength.
- Morning stiffness.
- Difficulty extending the wrist.
- Medical examination: the recognition of symptoms must NOT be aimed at self-management of the therapy, but at understanding the extent of the disorder. The diagnosis will be made by the orthopedist or, more rarely, by the general practitioner. To confirm the suspicion of the functional examination (palpation, Cozen test, Millis test) and perform a differential diagnosis, the specialist will prescribe some investigations such as:
- Radiography and ultrasound: they offer an "image (albeit of poor quality) of the inflamed tendons.
- X-rays: to rule out arthrosis and elbow arthritis or any tendon calcifications.
- Cervical magnetic resonance: to rule out a herniated disc.
- Electromyography (EMG): to rule out nerve compressions.
- With a positive diagnosis, the orthopedist will start the non-surgical treatment (resolving in 80-90% of cases):
- Total rest for several weeks:
- Initially forced by a splint or plaster.
- Subsequently dependent on the will of the subject, who must avoid any unnecessary or unscheduled solicitation.
- Anti-inflammatory drug therapy.
- For tennis players: suitable sports equipment (less rigid racket, less tight strings, shock absorbers) etc.
- Rehabilitation therapy: of physiotherapy extraction, it serves to strengthen the muscles of the forearm.
- Medical treatments: technological (shock waves, ultrasounds, tecar, etc.), cryotherapy (if the compromise concerns the muscle portion) or heat therapy (if the damage is exclusively to the tendons) depending on the case.
- Use of braces: for example elbow pads; they are a palliative but may lessen symptoms.
NB: If the epicondylitis affects both the muscles and the tendons, between that with heat and cryotherapy it is advisable to prefer cryotherapy.
- When necessary, resort to surgery (see below Medical Treatments).
- In chronic epicondylitis, complicate, destroy (with urinary waves) or surgically remove any tendon calcifications.
What NOT to do
- Do not adopt any preventive rules, especially if there is a clear predisposition to relapse.
- Ignore the symptoms, especially in the presence of a significant medical history.
- Do not seek medical attention and try to treat the condition by taking over-the-counter anti-inflammatory drugs.
- Do not perform diagnostic investigations for epicondylitis.
- Do not perform diagnostic investigations to exclude pathologies that can cause symptoms similar to epicondylitis.
- Using, loading or even overloading the already compromised elbow.
- Do not adopt the prescribed anti-inflammatory drug therapy.
- At the time of recovery, early use of equipment that can exacerbate the disorder.
- Do not follow rehabilitation therapy.
- Do not take advantage of technological healing methods, if recommended.
- Exclude a priori the possibility of surgery.
- If the epicondylitis continues to occur repeatedly, eliminate the activity responsible for the acute.
What to eat
There is no diet designed to prevent and heal epicondylitis better or faster.
However, some tricks may prove useful:
- Increase the intake of anti-inflammatory molecules:
- Omega 3: they are eicosapentaenoic acid (EPA), docosahexaenoic (DHA) and alpha linolenic (ALA). They have an anti-inflammatory role. The first two are biologically very active and are found mainly in: sardines, mackerel, bonito, sardinella, herring , alletterato, tuna belly, garfish, seaweed, krill etc. The third is less active but constitutes a precursor of EPA; it is mainly contained in the fat fraction of certain foods of vegetable origin or in the oils of: soy, linseed, seeds of kiwi, grape seeds etc.
- Antioxidants:
- Vitamins: the antioxidant vitamins are carotenoids (provitamin A), vitamin C and vitamin E. Carotenoids are contained in vegetables and red or orange fruits (apricots, peppers, melons, peaches, carrots, squash, tomatoes, etc.); they are also present in crustaceans and milk. Vitamin C is typical of sour fruit and some vegetables (lemons, oranges, mandarins, grapefruits, kiwis, peppers, parsley, chicory, lettuce, tomatoes, cabbage, etc.). Vitamin E can be found in the lipid portion of many seeds and related oils (wheat germ, corn germ, sesame, kiwi, grape seeds, etc.).
- Minerals: zinc and selenium. The first is mainly contained in: liver, meat, milk and derivatives, some bivalve molluscs (especially oysters). The second is mainly contained in: meat, fish products, egg yolk, milk and derivatives, enriched foods (potatoes, etc.).
- Polyphenols: simple phenols, flavonoids, tannins. They are very rich: vegetables (onion, garlic, citrus fruits, cherries, etc.), fruit and relative seeds (pomegranate, grapes, berries, etc.), wine, oil seeds, coffee, tea, cocoa, legumes and whole grains, etc.
What NOT to Eat
- The only group of foods (or better drinks) not recommended in case of epicondylitis is that of alcoholic beverages. Ethyl alcohol exerts a diuretic action and interferes with the metabolism by altering the efficacy of the active ingredients.
- Furthermore, we remind you that an excess of omega 6 fatty acids "could" have a diametrically opposite effect to the "intake of omega 3." It is good practice to limit the introduction of foods rich in linoleic, gamma-linolenic, diomo-gamma-linolenic acid and arachidonic They are mainly contained in: seed oil (especially peanuts), most of the dried fruit, certain legumes, etc.
Natural Cures and Remedies
- Stretching: Stretching can be static or dynamic, active or passive. For epicondylitis it has a preventive but also a therapeutic role in the chronic phase of treatment.
- Physiotherapy massage, osteopathic manipulations, cyriax and myofascial manipulations, diacutaneous myofibrolysis (see below Medical Treatments).
- Motor exercises for strengthening: used both in conservative therapy and in rehabilitation after surgery.
- Cryotherapy: cold therapy is useful in reducing pain and muscle inflammation. It should be performed 2 or 3 times a day. Ice should not be applied directly; on the contrary, it should be placed in a containment bag with water and applied by placing a woolen cloth to protect the skin.
- Warm compresses: They increase blood flow and can speed up the recovery of tendon injuries. They should not be used in the presence of vascular lesions.
- Braces, bandages and bandages: these are tools that are sometimes useful for the reduction of symptoms. They have the function of absorbing shocks and accompanying movement. In sports practice they cannot be very tight; on the contrary, during work it is possible to tighten them more vigorously, taking care not to compromise circulation.
Pharmacological treatment
- Analgesics: They are used to reduce pain. They are taken orally.
- Paracetamol: for example Tachipirina ®, Efferalgan ® and Panadol ®.
- Non-steroidal anti-inflammatory drugs (NSAIDs):
- Systemic for oral use: they are more used than topical ones, as the structures affected by inflammation are difficult to reach with skin application. They are more potent even if generic than ointments and gels. They may require the use of a gastroprotector. People with liver or kidney disorders are not always able to take them.
- Ibuprofen: e.g. Brufen ®, Moment ®, Spidifen ®, Nurofen ®, Arfen ®, Actigrip fever and pain ® and Vicks fever and pain ®).
- Ketoprofen: for example Arthrosilene ®, Orudis ®, Oki ®, Fastum gel ®, Flexen "Retard" ® and Ketodol ®.
- Diclofenac: for example Dicloreum ®, Deflamat ®, Voltaren Emulgel ® and Flector ®.
- Naproxen: for example Momendol ®, Synflex ® and Xenar ®.
- For topical use: they are mainly ointments or gels. They have the advantage of acting locally without straining the stomach and liver; however they are less effective. It must be specified that this is not the most suitable pharmacological category and persisting with their use (albeit in the initial stages) could favor the worsening of the inflammation.
- Ibuprofen 10% lysine salt or 2.5% Ketoprofen (for example Dolorfast ®, Lasonil ®, Fastum gel ® etc.).
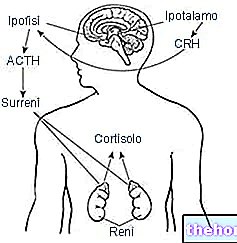
- Corticosteroids:
- Injectable by infiltration: they are used only if oral NSAIDs are not well tolerated due to: allergy, gastric ulcer, diabetes, etc. If used for long periods they have many side effects on the connective tissues. They are the most drastic but also the most effective pharmacological solution:
- Methylprednisolone: for example Depo-Medrol ® in combination with lidocaine (a local anesthetic).
Prevention
- Heating: has the function of warming the muscles and tendons of the elbow, increasing the elasticity and functionality of the structures involved.
- When approaching a new sport (tennis, baseball, rackets, etc.) it is advisable to gradually increase the intensity of the effort.
- Stretching and joint mobility: they are controversial and less effective than other body areas. To be practiced at rest from intense activity but ALWAYS HOT, they are of primary importance in increasing elasticity and ability to move. However, recent studies have not found a correlation with the reduction of joint injuries.
- In the event of a pre-existing injury, the use of functional bandages or special braces has proved to be quite useful in reducing the risk of recurrence.
Medical Treatments
- Physiotherapeutic massage, passive stretching and osteopathic manipulations: manual therapies can improve epicondylitis inflammation by relaxing contracted muscles (potentially responsible for the onset of epicondylitis and difficulty in healing).
- Cyriax and myofascial manipulations: eliminate the fibrosis that can form during the healing process in the tissues. They are especially indicated when epicondylitis is associated with impairments of muscles as well as tendons.
- Diacutaneous myofibrolysis: also aimed at counteracting the fibrosis localized in the trigger points. It exploits the mechanical action exerted by manual pressure of instruments called fibrolysers.
- Shock waves: they can accelerate healing if the damage is to the soft tissues. They are based on the localized release of acoustic impulses. The effect is an increase in the metabolic activity of the target tissue and the rupture of any tendon calcifications manifested in the chronic (rarer) forms.
- Laser therapy: it is a treatment that uses electromagnetic rays directly on the affected area. The electron beam from the laser acts on the cell membrane and mitochondria, increasing metabolic activity, reducing pain and inflammation, creating vasodilation and increasing lymphatic drainage.
- Tecar therapy: therapeutic method that uses an electric capacitor to treat joint muscle injuries. The mechanism of tecar therapy is based on the restoration of the electrical charge in the injured cells to ensure that they regenerate more quickly.
- Kinesio taping: exploits the traction of adhesive and elastic bandages which sometimes contain small pharmacological concentrations of anti-inflammatories. They should have a draining, slightly pain-relieving-anti-inflammatory and bracing function.
- Surgery: used only after 6-12 months from the beginning of conservative therapies with unsuccessful outcome. It almost always involves the removal of the diseased part of the muscle and reinserting it on the bone. It is carried out mainly in the open and more rarely in arthroscopy.
- Post-surgical rehabilitation: starts after about 7 days. At the eighth week we proceed with the strengthening and after 6 months it will be possible to return to the overload activities.