Edited by Dr. Stefano Casali
Control over the state of constriction or dilation of the vessels can only be exercised on structures with smooth muscles in their thickness. This control can be of nervous, hormonal and metabolic origin, therefore remote or local control. According to the importance or physiological characteristics of the perfused organ, all the circulatory districts will have the prevalence of one mechanism of action over another. In the capillaries, lacking a muscular tunic, the state of the walls is strictly dependent on the precapillaric sphincters, but above all on the transmural pressure.
Vessel Nervous Control
Vasoconstriction of nervous origin depends on the action of the sympathetic adrenergic vasoconstrictor which, acting on the musculature through a chemical mediator (noradrenaline), induces vasoconstriction. The action of the sympathetic vasoconstrictor system is constant, so much so that it is considered responsible for the vascular tone, but specifically on the arteries it is responsible for determining the diastolic pressure, acting directly on the peripheral resistance; through the containment vessels, veins and sinuses, of the venous return. It does not appear to act on the cephalic system.
- the fibers originate from the intermediate-lateral columns of the T1-L4 tract, exiting in the form of white communicating branches, enter the constitution of the sympathetic ganglionic chain, to enter the constitution of the afferent nerves.
Vasodilation can be passive, in this case dependent on the inhibition of the sympathetic adrenergic, or active with direct or indirect action.
- Live: the stimulation of a sensory nerve induces the production of kinins, as in the case of the vasodilation of the exocrine glands by cholinergic action. Also the production of kallikrein-kallidin-bradykinin as in the specific case of stimulation of the cord nerve of the eardrum with action on the submaxillary gland.
- Direct: based on the action of mediators such as acetyl-choline, dopamine, histamine, etc. on the vascular musculature. It can be of sympathetic or parasympathetic origin, and often the two systems integrate as in the case of the erigentes nerves, where the removal of the S2-S4 tract, origin of the autonomic system fibers, does not compromise the erection but only the reflex one derived from stimulation of the glans.
The direct vasodilating action does not intervene in the reflex regulation of pressure by stimulation of the baros and chemoceptors, and has no decisive action in the cephalic district. A characteristic, but entirely hypothetical, action is attributed to the cholinergic sympathetic system on the skeletal muscles following a hypothalamic stimulation, evidenced by a diffuse vasodilation noted in states of high stress.
Axonic reflex: it is a reflex type response, mediated by C neurons, following stimulation of the peripheral stump of a sensory nerve, therefore without involving the spinal centers, which causes vasodilation. The impulse therefore proceeds centrally to carry the pain information, centrifugally to induce vasodilation. This mechanism underlies the skin's triple response.
Catecholamines
Noradrenaline: acts exclusively as a vasoconstrictor, both as a mediator of the sympathetic and for intra-arterial infusion.
Adrenaline: it is vasoconstrictor in the spleen, kidney and skin, vasodilator for the coronary circulation, liver and skeletal muscles. High amounts of adrenaline produce generalized vasoconstriction, as it also interacts with alpha receptors. In any case, the effect of circulating catecholamines is decidedly less than that mediated by the sympathetic.
Alpha receptors: they interact only with noradrenaline, and are almost absent in the heart where they have a positive inotropic effect. Present in large quantities in the vascular smooth muscles.
Beta1 receptors: they interact with both catecholamines in the heart inducing chronotropic, domotropic and positive inotropic effects by increasing the mobility of calcium ions, such as the receptors described above.
Beta2 receptors: they are present in the liver, heart, and skeletal muscle, absent in the kidney, spleen, and skin.
Angiotensin: synthesized in systemic hypotension, derivative of angiotensinogen by the action of renin, has action only on resistance vessels and has a short duration.
Vasopressin: produced by the supraoptic nuclei of the ant. hypothalamus, it has a systemic antidiuretic and vasoconstrigent action, acting on the precapillaric sphincters, on the resistance vessels, but also on the venules.
Autacoids
Histamine: contained in the mast cells, is released following trauma, causing arteriolar vasodilation, vasoconstriction of the local venous district, increasing capillary permeability. In the skeletal muscle they are also released due to a decrease in orthosympathetic tone.
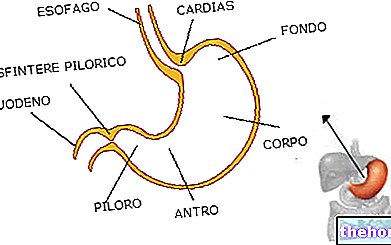
Serotonin: freed from aggregating platelets, they cause vasoconstriction of the injured vessel. In the stomach their secretion is caused by gastrin; they block adrenergic receptors, causing arteriolar vasodilation, and venular constriction to increase the availability of interstitial fluid.
Vasodilating metabolites:
Systemic hyperemia cannot be attributed to single ions or metabolites, but to a whole which, in any case, always follows the physiology of the tissue to be perfused. Ions potassium, calcium, but above all variations in the partial pressure of oxygen, or hypercapnia, unaccompanied however, an increase in blood flow are the most frequent cause of metabolite-induced vasodilation. Evidently these systems have a local action. nervous: in fact the ortho-para-sympathetic system is at the base of the heart tone, while in the circulatory there is only a constricting tone of orthosympathetic origin. The dilation is attributable on a reflex basis to inhibition of the vessel-motor. Only some areas can be forced by the "action of" adrenaline.
Integrated body pressure regulation system:
A few seconds:
- Baroceptive System
- Ischemic mechanism of the CNS
- Mechanism of Chemoreceptors
Seconds to minutes:
- Renin-Angiotensin system
- Stress-relaxation mechanism
- Mechanism of liquid movement through the Capillaries
Minutes to infinity:
- Kidney-liquid system integrated by the Renin-Angiotensin-Aldosterone system
Bibliography:
- Stagnaro-Neri M., Stagnaro S., Biophysical Semeiotics: evaluation of arterial compliance and peripheral arterial resistance. Acts of the XVII Cong. Nat. Soc. Ital. Microcirculation Studio, Florence Oct. 1995, Biblioteca Scient. Military Health School, 2, 93.
- Pfeifer JR. The anatomy and physiology of the venous system of the lower extremities. Ed Phlebologle, 1992.
- Braundawall E. Heart Diseases: Treatise on cardiovascular medicine. Ed. Piccin.
- Hayashi K.. Experimental approaches on measuring the mechanical properties and constitutive laws of arterial walls, Journal of Biomechanical Engineering, Vol. 115.
- Testut L.. Human Anatomy, fourth book: Angiology.
- ATM. Atlas text - Fundamental concepts. Rampello A.
- Taglietti-Box "Principles of Physiology", The Goliardica Pavese.
- Silverthorn "Physiology", Ambrosiana Publishing House.
- De Trafford J. C., Lafferty K., Kitney R. I., Cotton L. T., Roberts V. C. Modeling of the human vasomotor control system and its application to the investigation of the arterial disease. IEEE Proc. 129A, 1982.
- Green J. H. Introduction to human physiology. Zanichelli, 1972.
- Guyton A. C. Treatise on medical physiology. II Italian edition on the V American edition by prof. Alfredo Curatolo, Piccin Nuova Libraria, Padua, 1987.
- Montano N., Gnecchi Ruscone T., Porta A., Lombardi F., Pagani M., Malliani A. Power spectrum analysis of heart variability to asses the changes in sympathovagal balance during graded orthostatic tilt. Circulation, vol. 90, n ° 4, 1994.
- Burton A. C. Physiology and biophysics of circulation. An introductory text. Italian ed. By dr. Franco Tripodi, The Scientific Thought Publisher, Rome, 1983.