Glycogen is a macromolecule (molecular mass of about 400 million daltons) of α-glucose in which there are mainly α-1,4 glycosidic bonds and ramifications in a ratio of 1:10, due to α-1,6 glycosidic bonds.
Glycogen constitutes reserve material and is continuously degraded and reconstituted; in the whole body cell mass, there are about 100 g of glycogen: most of it is in the liver where it is mobile and can, therefore, be used as a reserve for other organs (glycogen in muscles is not mobile).
The enzymes that catalyze the degradation and synthesis of glycogen are all in the cytoplasm, therefore a regulation system is needed that makes one path inactive when the other is active: if there is glucose available, the latter is converted into glycogen (anabolism) which is a reserve, vice versa, if c "is required for glucose, then the glycogen is degraded (catabolism).

The enzyme mainly involved in the breakdown of glycogen is the glycogen phosphorylase; this enzyme is able to cleave a glycosidic α-1,4 bond using, as a lytic agent, an inorganic orthophosphate: the cleavage occurs by phosphorolytic way and glucose 1-phosphate is obtained.
At five or six units from a branching point, the glycogen phosphorylase enzyme is no longer able to act so it detaches from the glycogen and is replaced by a deramifying enzyme which is a transferase: in the catalytic site of this enzyme c "is a" histidine that allows the transfer of three saccharide units to the nearest glycosidic chain (histidine attacks the first carbon of a glucose molecule). The enzyme just mentioned is the glycosyltransferase; at the end of the action of this enzyme, only one glucose unit remains on the side chain with the first carbon bound to the sixth carbon of a glucose in the main chain. The last glucose unit in the side chain is released by the action of "enzyme α-1,6 glycosidase (this enzyme constitutes the second part of the deramifying enzyme); given that the branches in glycogen are in a ratio of 1:10, from the complete degradation of the macromolecule we obtain about 90% of glucose 1-phosphate and about 10% of glucose.
The action of the aforementioned enzymes allows the elimination of a side chain from the glycogen molecule; the activity of these enzymes can be repeated until complete degradation of the chain occurs.
Let's consider a hepatocyte; glucose (assimilated through the diet), when it enters the cell is converted to glucose 6-phosphate and thus is activated. Glucose 6-phosphate, by the action of phosphoglucomutase, is transformed into glucose 1-phosphate: the latter is a non-immediate precursor of biosynthesis; in biosynthesis an activated form of sugars is used which is represented by sugar linked to a diphosphate: usually uridyldiphosphate (UDP). Glucose 1- phosphate is then converted into UDP-glucose, this metabolite under the action of glycogen synthase which is able to bind UDP-glucose to a non-reducing end of the growing glycogen: elongated glycogen of a glucosidic unit and UDP are obtained. UDP is converted by the nucleosided diphosphokinase enzyme into UTP which returns to the circulation.
The degradation of glycogen occurs by the action of glycogen phosphorylase which releases a molecule of glucose and transforms it into glucose 1-phosphate. Subsequently, phosphoglucomutase converts glucose 1-phosphate to glucose 6-phosphate.
Glycogen is synthesized, above all, in the liver and muscles: in the organism there is 1-1.2 hectograms of glycogen distributed throughout the muscle mass.
The glycogen of a myocyte represents an energy reserve only for this cell while the glycogen contained in the liver is also a reserve for other tissues, that is, it can be sent, as glucose, to other cells.
The glucose 6-phosphate obtained in the muscles from the degradation of glycogen is then sent, in case of energy requirement, to glycolysis; in the liver, glucose 6-phosphate is converted into glucose by the action of glucose 6-phosphate phosphatase (enzyme characteristic of hepatocytes) and is conveyed into the bloodstream.
Glycogen synthase and glycogen phosphorylase both work on the non-reducing units of glycogen so there must be a hormonal signal that commands the activation of one pathway and the blocking of the other (or vice versa).
In the laboratory it was possible to lengthen the glycogen chain by exploiting glycogen phosphorylase and using glucose 1-phosphate in a very high concentration.
In cells, glycogen phosphorylase only catalyzes the degradation reaction because the concentrations of the metabolites are such as to shift the equilibrium of the following reaction to the right (ie towards the degradation of glycogen):

Let's see the mechanism of action of glycogen phosphorylase: the acetal oxygen (which acts as a bridge between the glucose units) binds to the hydrogen of the phosphoryl: a reaction intermediate is formed given by a carbocation (on the glucose which is all " extremities) to which phosphoryl (Pi) binds very quickly.
Glycogen phosphorylase requires a cofactor which is pyridoxal phosphate (this molecule is also a cofactor for transaminases): it has a partially protonated phosphoryl (pyridoxal phosphate is surrounded by a hydrophobic environment which justifies the presence of protons bound to it) . The phosphoryl (Pi) is able to transfer a proton to the glycogen because this phosphoryl then reacquires the proton from the partially protonated phosphoryl of the pyridoxal phosphate. The probability that, at physiological pH, the phosphoryl will lose the proton and remain completely deprotonated is very low.
Now let's see how phosphoglucomutase works. This enzyme presents, in the catalytic site, a residue of phosphorylated serine; serine yields phosphoryl to glucose 1-phosphate (in position six): glucose 1,6-bisphosphate is formed for a short time, then serine is rephosphorylated taking the phosphoryl in position one. Phosphogluco mutase can work in both directions, ie converting glucose 1-phosphate into glucose 6-phosphate or vice versa; if glucose 6-phosphate is produced, it can be sent directly to glycolysis, in the muscles, or transformed into glucose in the liver.
The enzyme uridyl phosphogluco transferase (or UDP glucose pyrophosphorylase) catalyzes the glucose 1-phosphate transfer reaction to UTP by attachment to phosphoryl a.
The enzyme just described is a pyrophosphorylase: this name is due to the fact that the opposite reaction to the one just described is a pyrophosphorylation.
UDP glucose, obtained as described, is able to lengthen the glycogen chain, by a monosaccharide unit.
It is possible to make the reaction evolve towards the formation of UDP glucose by eliminating a product which is pyrophosphate; the enzyme pyrophosphatase converts pyrophosphate into two molecules of orthophosphate (hydrolysis of an anhydride) and in so doing, keeps the concentration of pyrophosphate so low as to make the process of formation of UDP glucose thermodynamically favored.
As mentioned, UDP glucose, thanks to the action of glycogen synthase, is able to lengthen the glycogen chain.
The ramifications (in a ratio of 1:10) are due to the fact that, when a glycogen chain consists of 20-25 units, a branching enzyme (having a "histidine on its catalytic site) intervenes, capable of transferring a series of 7 -8 glycosidic units further downstream of 5-6 units: thus a new branching is generated.
For reasons of nervous origin or if energy is needed due to physical exertion, adrenaline is secreted from the adrenal glands.
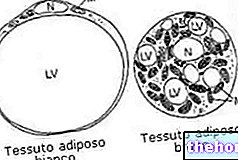
The target cells of adrenaline (and noradrenaline) are those of the liver, muscles and adipose tissue (in the latter there is the degradation of triglycerides and the circulation of fatty acids: consequently, glucose is produced in the mitochondria 6 -phosphate, to be sent to glycolysis, while in adipocytes, glucose 6-phosphate is transformed into glucose by the action of the enzyme glucose 6-phosphate phosphatase and exported to the tissues).
Let's see, now the modalities of action of adrenaline. Adrenaline binds to a receptor placed on the cell membrane (of myocytes and hepatocytes) and this determines the translation of the signal from outside to inside the cell. The protein kinase is activated which acts simultaneously on the systems that regulate synthesis and degradation of glycogen:
Glycogen synthase exists in two forms: a dephosphorylated (active) form and a phosphorylated (inactive) form; protein kinase phosphorylates glycogen synthase and blocks its action.
Glycogen phosphorylase can exist in two forms: an active form in which a phosphorylated serine is present and an inactive form in which serine is dephosphorylated. Glycogen phosphorylase can be activated by the enzyme glycogen phosphorylase kinase. Glycogen phosphorylase kinase is active if it is phosphorylated and inactive if it is dephosphorylated; the protein kinase has as substrate the glycogen phosphorylase kinase, that is, it is able to phosphorylate (and, therefore, activate) the latter which, in turn, activates the glycogen phosphorylase.
Once the adrenaline signal is over, the effect it has on the cell must also end: phosphatase enzymes then intervene on the protein species.