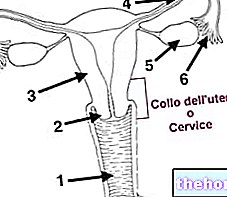
The wall of the uterus is made up of three layers of tissue, which from the inside outwards are called:
- endometrium: mucous membrane that lines the uterine cavity internally
- myometrium: muscular tunic, consisting of a layer of smooth muscle which contributes 90% c.a. to the overall thickness of the organ
- perimetry: serous tunic, peritoneal sheet that covers it externally only in the body and in the bottom (missing in the sides and in the supravaginal portion of the cervix)
Before going into the description of the endometrium, let us briefly recall how in the uterus, from a macroscopic point of view, four different regions are identified:
- body of the uterus: upper portion, more expanded and voluminous
- neck of the uterus or cervix: lower portion, smaller and narrower, about 3-4 cm long. Turned downwards, it looks towards the vagina where it protrudes through the so-called "tench snout".
- isthmus of the uterus: narrowing that divides the body and neck of the uterus
- fundus or base of the uterus: portion of the uterine cavity located above the imaginary line that joins the two fallopian tubes, facing forward
Endometrium: histology
The endometrium internally lines the walls of the uterus. It therefore represents the innermost layer of the organ, facing the lumen or uterine cavity, which rests directly on the underlying musculature (myometrium)
As we will see better in the next chapter, in women of childbearing age the endometrium has a thickness of 1-7 mm depending on the phase of the menstrual cycle. The endometrium is made up of two layers that differ in structure and function: a layer deeper basal and a superficial layer represented by the superficial epithelium, the endometrial glands and the stroma.
- Coating epithelium cylindrical (syn. Batiprismatic or columnar) simple (syn. Monostratified) ciliated; it is composed of a single layer of hair cells, interspersed with mucus-secreting goblet cells. The hair cells cause a direct flow to the cervix
- Proper tunic (lamina) or stroma, formed by loose connective tissue poor in fiber and rich in vessels and glands, mostly tubular and simple, which produce a secretion rich in glycoproteins and glycogen. It is a highly vascularized functional layer, which varies in thickness during the various phases of the cycle and can provide the implant bed for the blastocyst (fertilized egg cell). The deepest part constitutes the so-called basal layer, very thin and insensitive to hormones. , which adheres to the underlying myometrium.
The cervical canal has a different mucosa from the endometrium in function and structure. In the cervix the endometrium is not as smooth as the overlying areas, but rises in folds that make up the arbor vitae. In the lower part of the cervix (exocervix) the lining epithelium - passing through a so-called transformation zone - from simple cylindrical ciliated to multi-layered pavement (squamous) devoid of glands, similar to the vaginal one

- Straight arteries that cross the myometrium, reach the proper tunic and capillarize in the depths of the endometrium.
- Spiral-shaped arteries that once crossed the myometrium enter the endometrium taking a tortuous course until they reach under the lining epithelium where they give rise to capillarization.
Based on the distribution of these vessels, the endometrium of a woman of childbearing age is distinguished in:
- Basal area: very thin, close to the myometrium, contains the bottom of the uterine glands, the capillarization of the straight arteries and the trunk of the spiral-shaped arteries
- Functional zone: above the basal, it contains the body of the uterine glands, the body of the spiral-shaped arteries with their most tortuous portion, and more on the surface also the lining epithelium. The functional zone therefore contains the ciliated lining epithelium and the more superficial layers of the lamina propria.
These two areas respond differently to female sex hormones; in fact, the basal area does not undergo cyclical changes, while the functional area is subject to periodic changes based on the levels of estrogen and progesterone. The basal zone therefore represents the layer from which, after menstruation, the previously lost functional zone is restored.
Before menstruation, during the so-called secretory phase, three layers are recognized in the endometrium of the body and fundus.
- compact: most superficial layer, contains the neck of the glands
- spongy or spongy: organized in a looser way, it contains the basal portion of the glands
functional area
- basal: very thin layer that rests on the underlying uterine myometrium; contains the bottom of the uterine glands and is devoid of estrogen and progesterone receptors, therefore it is not sensitive to the action of ovarian steroids
basal zone
While the fundus and body endometrium undergoes continuous functional changes between the beginning of one menstruation and the end of the next, the mucous membrane of the neck does not undergo the same cyclical changes.


Endometrium: what are its functions?
In addition to representing the innermost layer of the organ, the endometrium is also the most dynamic tissue of the uterus.
From puberty (11-13 years) to menopause (45-50 years), the endometrium of the body and fundus undergoes cyclical and massive changes, which occur every 28 days (approximately) under the influence of ovarian hormones. :
- regenerative and proliferative phase (days 5-14): the uterine endometrium is gradually enriched with new cells and blood vessels, the tubular glands lengthen and overall the endometrium increases its thickness
- glandular or secretory phase (days 14-28): in this phase the endometrium reaches its maximum thickness, the cells enlarge and fill with fat and glycogen, the tissue becomes edematous → the uterus is functionally and structurally ready to accommodate the cell fertilized egg and to support it in its development.
- desquamative or menstrual phase (days 1-4): the constant maintenance of the endometrium in a state favorable to implantation would be, for the organism, too expensive from an energy point of view. For this reason, if the egg cell does not is fertilized, the most superficial layer of the endometrium undergoes apoptosis, flaking off; the leakage of small quantities of blood and tissue residues by now dead gives rise to the menstrual flow.

PLEASE NOTE: at the level of the neck of the uterus, the mucosa does not undergo cyclical changes as striking as those described above. What varies is above all the mucous secretion of the cervical glands:
- generally very dense, to the point of forming a real plug that hinders the ascent of spermatozoa in the neck of the uterus, in the days between ovulation, it undergoes a fluidification, becomes stringy, watery, acellular, alkaline and easily penetrable by the spermatozoa
The mucous secretion of the uterine cervix also protects the innermost genital organs from ascending infections.
Pathologies of the endometrium
- Endometriosis
- Endometrial cancer




.jpg)


















