- Most of the bilirubin (85%) comes from the normal process of destroying exhausted red blood cells. These cells have a life of about 120 days: first they are degraded by the spleen and are incorporated in the biliverdin, then the residues are transported to the liver to be metabolized.
- The rest of the bilirubin comes from the bone marrow or the liver.
Under normal conditions, all the bilirubin that originates from hemoglobin is eliminated by a mechanism that is usually found in equilibrium: what is produced is also processed to be degraded. However, if you notice a yellowish tint to the skin and eyes, we are faced with a clinical condition - caused by high circulating bilirubin - called jaundice.
The bilirubin test measures its concentration in the blood to evaluate liver function or to diagnose anemia caused by damage or breakdown of red blood cells (haemolytic anemia).
or be intercepted by macrophages of the spleen. In both cases, the body cannot afford the luxury of wasting some of their constituents, first of all the iron contained in the prosthetic group EME (which represents the oxygen-binding heart of hemoglobin).The recycling operations take place above all at the level of the spleen, where the waste molecules are incorporated in a green pigment, called BILIVERDINA, which is readily converted into bilirubin.
Bilirubin, yellow-orange in color and not reusable, must be eliminated; to do this, the body must first of all make it acquire solubility in water; for this reason it is transported in the bloodstream by a specific carrier, in this case albumin.
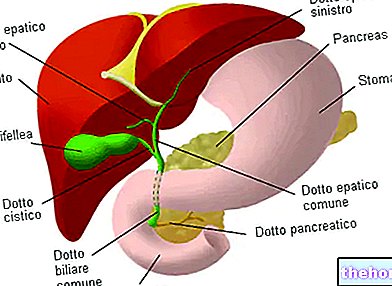
Plasma albumin carries bilirubin to the liver, which helps make it water-soluble by combining it with glucuronic acid and transforming it into bilirubin diglucuronide, also known as direct bilirubin or conjugated bilirubin. Instead, we speak of indirect bilirubin to indicate the amount of bilirubin that must still be processed by the liver.

Unconjugated bilirubin, not being water-soluble, cannot be filtered by the kidney, so it is not found in the urine. However, due to its high fat solubility, once it has been separated from the albumin, it can easily penetrate into the tissues.
The ratio between direct bilirubin and indirect bilirubin, which varies on average between 1: 4 and 1: 5, constitutes a very important, and therefore widely used, diagnostic criterion for evaluating liver function.
The amount of total bilirubin (deriving from the sum of these two fractions), produced daily, is around 250 mg and reaches an average concentration of 1-1.5 mg / dL in the blood.
Blockage or deficiency of bilirubin excretion mechanisms leads to its accumulation in the blood (hyperbilirubinemia) and tissues, inducing a condition, known as jaundice, in which the skin is yellow in color.