Blood pressure regulation
When the heart's ventricle contracts, blood is pushed into the large arteries; here, the presence of elastic and muscular tissue facilitates its progression and helps regulate its flow. The pressure impressed on the blood mass stretches the arterial walls, which accumulate elastic energy to be released in the subsequent diastole phase (ventricular relaxation). The energy accumulated during systole is then slowly transferred to the blood column directed to the periphery; in this way the arteries help to transform the intermittent blood flows, coming from the heart, into a continuous (laminar) flow, essential to allow normal exchanges to capillary level.
If the walls of the arteries were rigid, the systolic pressure would rise rapidly, and then leave room for an "equally sharp drop in the diastolic phase. This is why aging and various pathological stages (such as atherosclerosis) bring with them a loss of vascular elasticity and a consequent increase in blood pressure (hypertension).
The district regulation of blood flow is entrusted above all to the arterioles which, thanks to the rich muscular tunic, can contract and decrease their lumen until it closes, or release and increase it. During physical exercise, for example, the arterioles of some districts are occluded, while those present in the muscular areas involved in physical effort dilate.
Main arteries of the human body
With a diameter of about 2 and a half centimeters, the maximum artery of the human body is the aorta, which emerges from the left ventricle of the heart, presenting itself as an uninterrupted trunk that tends to decrease only towards the end of its journey. the aorta takes on different names (ascending aorta, arch of the aorta, descending abdominal - thoracic aorta) and originates numerous vessels of lower caliber directed to different body districts. From the "arch of the aorta" the carotid and subclavian arteries branch off, directed, respectively, in the head and upper limbs; in the descending tract the celiac trunk is born - which supplies the stomach, spleen, liver and pancreas - the two mesenteric arteries (upper and lower that supply the intestine), and the renal arteries directed to the homonymous organs emunctors. At the height of the pelvis the descending branch of the aorta undergoes a branching, originating the two common iliac arteries, which, after originating the internal iliac arteries directed to the pelvis, continue in the lower limbs as femoral arteries.
Arteries generally run deep in the body (except in some regions: temples, wrists, neck), so much so that many skeletal segments receive imprints. The branches formed by the arteries are of two types: terminal, due to the bifurcation of an arterial trunk that ceases to exist (for example, the brachial or humeral artery, which splits into the radial and ulnar) and collateral, which detach from an "artery which then continues its course. The arterial vessels are connected to each other through frequent anastomotic trunks, a sort of natural bypass. Their presence guarantees - within certain limits - the vascularization of an organ or part of it even when an "artery is blocked. Arterial anastomoses are abundant in the abdominal organs, around the joints (where a movement can inhibit the flow in some channels ) and in the coronary area.
The arterioles
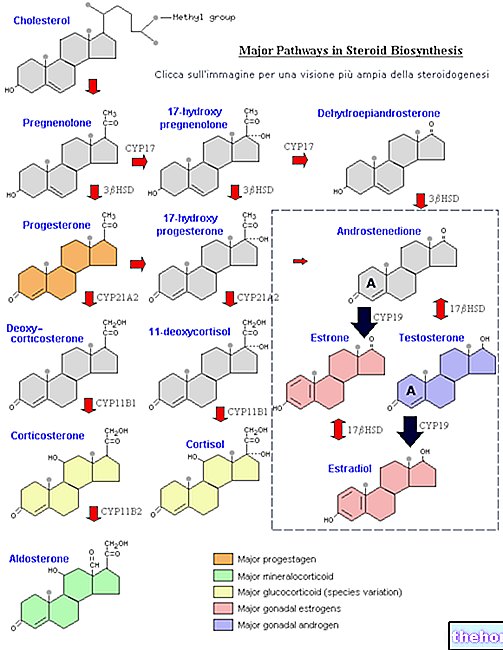
The resistance offered by the arterioles to the passage of blood is inversely proportional to their radius; in other words, the more they are dilated and the less resistance they offer. But what controls the contraction and relaxation of the anterior muscles? As anticipated, there are mechanisms mediated by sympathetic nerves (thanks to the release of noradrenaline), which regulate blood distribution to satisfy some homeostatic needs, such as temperature. There is also a local control, dependent on the metabolic needs of the tissue itself, and a hormonal control that mainly involves the hormones involved in the regulation of the excretion of water and salts by the kidney (see aldosterone, atrial natiuretic peptide and vasopressin). Another interesting mechanism of blood flow regulation is myogenic self-regulation, a phenomenon whereby the arterioles subjected to an increase in tension, a symptom of a rise in blood pressure, constrict themselves by decreasing the flow that passes through them.
Perhaps the most interesting aspect that regulates the contraction of vascular smooth muscle is the aforementioned local control. This mechanism involves the endothelium of the intimate tunic, which has the ability to release mediators of vasoconstriction and vasodilation, but also to activate platelets. , trigger an immune response and participate in the mechanisms of angiogenesis (development of new blood vessels starting from existing ones) and in vessel remodeling. Among these mediators, currently the subject of an intense study by researchers, we remember nitric oxide and nitrosyl radicals (vasodilators), endothelin and angiotensin II (vasoconstrictors); nitric oxide plays an important physiological role also in the reflex of the penis erection (see dedicated article).
The activity of the arterioles is also regulated by substances released by local cells, as well as by plasma levels of oxygen and carbon dioxide. With regard to the latter, it is clear that reduced oxygenation reflects the need for a greater blood flow, to be satisfied through the release of the arteriolar smooth muscle. In the same way, when the tissue oxygen supply drops significantly, the blood is enriched with carbon dioxide and H + ions; also the district metabolic acidosis represents a strong stimulus to arteriolar vasodilation.
The "metarterioles" begin immediately downstream of the arterioles; these vessels, provided with discontinuous smooth muscle, continue both with a certain number of capillaries and with "collateral" vascular pathways for regulatory purposes.
Physiology of the capillary circulation "






.jpg)


















