
Immunity is defined as the ability of an organism - congenital or acquired - to resist attack by pathogens and toxins. The ability of the immune system to induce an inflammatory process is essential for the restoration of biological functions and cell survival; however, this ability is not always beneficial. In fact, autoimmune pathologies or allergic reactions cause an anomalous recognition of external agents and excessive and altered inflammatory responses.
and capillary permeability;Each of these phases is modulated by chemical mediators: intercellular adhesion factors, pro-inflammatory cytokines, bradykinin, histamine, platelet aggregating factor, prostanoids (prostaglandins, thromboxanes and leukotrienes).
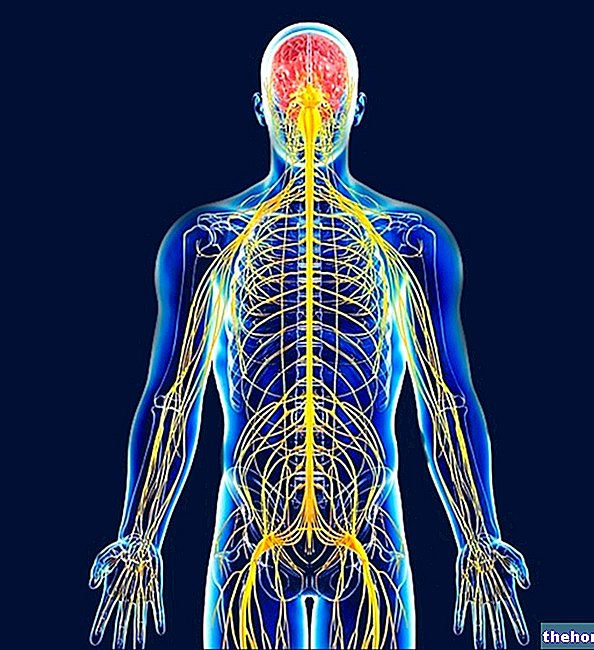
In general, the defense systems are divided into those that constitute innate (or non-specific) immunity and adaptive (or specific) immunity.
Innate immunity represents the first generic line of defense against all infectious agents and has the characteristic of being already present in the organism, therefore rapidly induced after exposure to the pathogen. Adaptive immunity, on the other hand, has the ability to specifically recognize and destroy the pathogen or products processed by it; it is activated in a longer time and gives the organism the memory of contact with a specific foreign pathogen.
It should be noted that the distinction between innate and acquired immunity is aimed only at the need to highlight the differences between the two defense systems, as it is now clear that these systems they do not operate separately but in concert, activating each other in order to amplify the immune response and make the destruction of the infectious agent effective.
What are the fates of the Inflammatory Response?
- A sudden response allows complete healing and restoration of tissues in physiological conditions;
- A delayed response induces scarring of the tissue lesion caused by the inflammation;
- An insufficient response induces a "chronic inflammation of the affected area", with the destruction of the tissue.
The adaptive reaction consists of a double response, a vascular one - characterized by vasodilation and capillary permeability with exudate leakage - and a cellular one, characterized by the release of chemical mediators that lead to the lysis of the pathogen. The non-specific response involves the recognition of the pathogen from part of the macrophages, which release interleukin-1 and interferon-α, adhere to endothelial cells and favor the adhesion of phagocytes. The phagocytosis process is favored by the opsonization of the pathogen, in other words, by the coating of the pathogen with opsonins (these are particular macromolecules which, if they cover the pathogen, increase the efficiency of phagocytosis as they are recognized by specific localized receptors. on the phagocyte membrane).
For further information: Natural Defenses Against Infections ) belonging to single foreign pathogens;Adaptive immunity is articulated in humoral - or antibody-mediated - immunity and in cell-mediated immunity, in which T lymphocytes intervene.
After the first encounter with the pathogen, the organism produces specific antibodies or cytokines against that particular pathogen, to specialize the defensive response. The production of antibodies or cytokines by lymphocytes occurs following the presentation of the antigen by APC cells (Antigen Presenting Cells), which engulf the infectious agent, digest it fragmenting it into short peptides and expose it on its surface. If, on the other hand, the infectious agent is intracellular in nature, the cytotoxic lymphocytes induce cell necrosis of the infected cells only.
To deepen the subject, read also: Immune SystemOther items that may interest you
- Inflammation and NSAIDs
- NSAIDs and Prostaglandins: what relationship?
- NSAIDs - Mechanism of Action, Indications and History
- NSAIDs - Classification and Choice
- NSAIDs: Unwanted Effects and Contraindications











.jpg)











