Edited by Dr. Stefano Casali
Anatomical factors
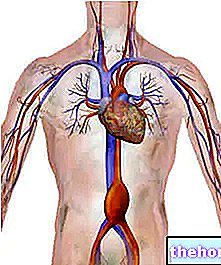
Coronary vessels can be divided into:
- conductance vessels (large epicardial branches and their branches)
- resistance vessels (intramyocardial branches and arterioles).
Coronary resistance is regulated by extrinsic factors (compressive action of the ventricular myocardium) and intrinsic factors (neurohormonal, myogenic and metabolic in nature).
Mechanical factors
- Coronary flow occurs mainly in diastole since in systole the intramural branches are virtually occluded by the ventricular contraction.
- It follows that tachycardia predisposes to the development of ischemia, since it shortens the time to diastole.
- The subendocardial layers are generally the most exposed to ischemia, above all because they are most exposed to endocavitary diastolic pressure.
Neurogenic factors
- The coronary arteries are innervated by the S.N.A.
- Stellate ganglion stimulation (orthosympathetic) causes vasodilation (mediated by Beta receptors) but at the same time increases contractility and heart rate. Beta receptor blockade induces the appearance of alpha-mediated effects (vasoconstriction).
Metabolic factors
- The increase in the metabolic demand of the myocardium determines hydrolysis of ATP and consequent release of adenosine in the interstitium.
- Adenosine induces vasodilation (antagonizing the entry of the calcium ion into the smooth muscle cells) especially at the level of the resistance vessels, with a consequent increase in coronary flow proportional to the increase in metabolic demands.
- Adenosine is not the only substance involved in the process (the eicosanoid system, the synthetetase nitroxide activity) but it is probably the main one.
Pathophysiology
There are two factors involved in the genesis of myocardial ischemia:
- The reduction of coronary flow.
- The increase in myocardial oxygen consumption (MVO2).
Reduction of coronary flow:
- In the event of an increase in metabolic demands, the coronary circulation is no longer able to cope with the demands with the onset of ischemia.
- Ischemia initially affects the subendocardial layers.
- A modulation of the coronary tone linked to neurohumoral factors can temporarily modify the coronary reserve; this explains the variability of the ischemic threshold which is usually observed in the clinic even in the same subject.
Determinants of myocardial O2 consumption:
The heart is an aerobic organ and, physiologically, the determination of the myocardial need for O2 provides an accurate index of its overall metabolism.
The main determinants of myocardial O2 consumption are:
- Heart rate.
- Contractility.
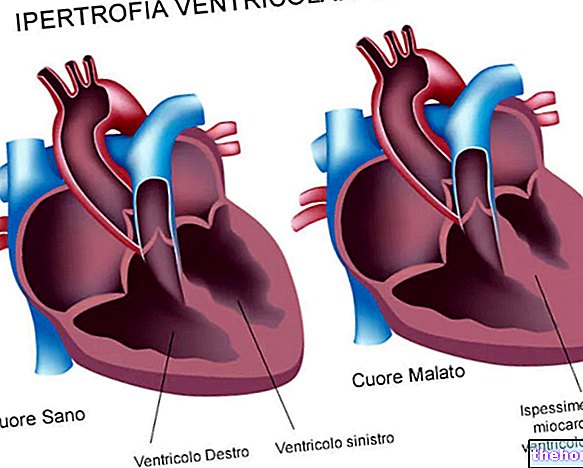
- Wall voltage.
Clinical manifestations
- Stable coronary syndromes: Angina due to exertion
- Acute (unstable) coronary syndromes: unstable angina, new onset angina, postinfarction angina, crescendo angina, Prinzmetal's variant angina (vasospastic).
Precipitating factors
- Attack provoked by an effort, in particular it can be triggered with a job that involves the use of the arms above the level of the shoulder.
- Cold environment, walking against the wind, walking after a big meal.
- Hypertensive crisis.
- Fear, anger, anxiety, emotional tension.
- Sexual intercourse.
Associated symptoms
- Shortness of breath, dizziness, palpitations, weakness.
Bibliography
Harrison .: Principles of Internal Medecine 12th ed. Mc Graw Hill 990.
Chierchia S., Brunelli C., Simonetti I. and Coll .: Sequence of events in angina at rest: primary reduction in coronary blood flow. Circulation, 61 : 1980.
Helfant R.H .: Stable angina pectoris: risk stratifications and therapeutic options. Circulation, 82: 1990.
Maseri A .: Pathogenetic mechanisms of angina pectoris: expanding views. Br. Heart. J., 43 : 1980.
Physiology of man, E. Di Prampero and A. Veicsteinas, Edi Ermes.
vom-Dahl J, Eitzman DT, al-Aouar ZR, et al. Relation of regional function, perfusion, and metabolism in patients with advanced coronary artery disease undergoing surgical revascularization. Circulation 1994; 90: 2356-2366.
Di-Carli MF, Asgarzadie F, Schelbert HR, et al. Quantitative relation between myocardial viability and improvement in heart failure symptoms after revascularization in patients with ischemic cardiomyopathy. Circulation 1995; 92: 3436-3444.
Berne & Levy, Cardiovascular Physiology, McGraw-Hill
Ades PA. Cardiac rehabilitation and secondary prevention of coronary heart disease. N Engl J Med 2001.
Dafoe WA, Lefroy S, Pashkow FJ et al. Programmodels for cardiac rehabilitation. In: Clinical CardiacRehabilita-tion: a cardiologist "s guide. Williams and Wilkins 1999.
Wannamethee SG, Shaper AG, Walker M. Physicalactivity and mortality in older men with diagnosedcoronary heart disease. Circulation 2000.
Box C. - Taglietti V. Principles of Physiology Volume I and II, La Goliardica Pavese, Pavia. Volume I, 1996.
Critical Patient in cardiovascular diseases. Roberto Torre, Cristiana Luciani, Susanna Sodo, September 2005.
Other articles on "Ischemic heart disease: pathophysiology"
- Coronary heart disease in short
- Ischemic heart disease
- Ischemic heart disease - Drugs for the treatment of ischemic heart disease
- Heart disease and metabolic disorders