Generality
What is an atheroma?
Atheroma, better known as atherosclerotic plaque, can be defined as a degeneration of the arterial walls due to the deposit of plaques formed essentially by fat and scar tissue.

Complications
An artery filled with lipid material and fibrotic tissue loses elasticity and resistance, is more susceptible to rupture and reduces its internal lumen, hindering blood flow. Furthermore, in the event of a rupture of the atheroma, reparative and coagulative processes are established which can lead to rapid occlusion of the vessel (thrombosis), or generate more or less severe embolisms if a fragment of the atheroma detaches and is pushed - like a stray mine - to the periphery, with the risk - if the fibrinolytic phenomena do not intervene in time - to obstruct a downstream arterial vessel.
In light of this description, it is well understood how atherosclerotic plaques - although asymptomatic even for decades - often give rise to complications, typically starting from late adulthood, such as: angina pectoris, myocardial infarction, stroke, gangrene.

Atheroma is the typical expression of a chronic inflammatory disease called atherosclerosis, the main cause of cardiovascular diseases which in turn - at least in industrialized countries - represent the leading cause of death among the population.
Structure of the arterial vessels
It is known to most people as a diet rich in (saturated) animal fats and cholesterol - together with overweight and obesity, smoking and a sedentary lifestyle - represents one of the main risk factors for atherosclerotic disease.
To understand how an atheroma is formed, it is first of all necessary to briefly brush up on the histology of the arterial walls, which are made up of three layers:
- the intimate, with its 150-200 micrometers in diameter, is the innermost or deepest layer of the vessel, the one in close contact with the blood; it is mainly made up of endothelial cells, which delimit the lumen of the vessel constituting the contact element between blood and arterial wall
- the medium tunic, 150-350 micrometers in diameter, is composed of smooth muscle cells, but also of elastin (which gives elasticity to the vessel) and collagen (structural component)
- the adventitia represents the outermost layer of the artery; 300-500 micrometers in diameter, it contains fibrous tissue and is surrounded by perivascular connective tissue and epicardial fat.
Atherosclerotic lesions mainly affect the large and medium arteries, where elastic tissue (especially in the large arteries) and muscle tissue (especially in the medium and small arteries) prevails. Furthermore, they tend to develop in predisposed regions, such as the branching points of the arteries characterized by a turbulent blood flow, sparing the adjacent segments. The atherosclerotic process begins very early, from adolescence (childhood obesity problem) or from early adulthood.
Biology of atheroma
The atherosclerotic process starts from the endothelial cells, then from the innermost layer of the arterial vessel.
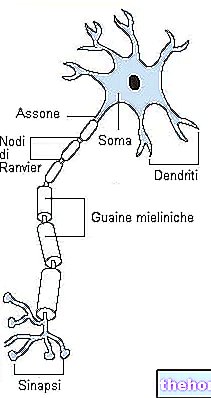
Considering the endothelial tissue as a simple lining of the vessels is very reductive, so much so that today the endothelium is considered a real organ, capable of processing many active substances capable of modulating the activity, not only of the various structures of the vessel wall. , but also of the blood cells and proteins of the coagulation system that come into contact with the surface of the endothelium. These active substances are partly released in the immediate vicinity (paracrine secretion), exerting their effects on the vessel wall, and partly released into the bloodstream (endocrine secretion), to carry out their action at a distance (e.g. nitric oxide and endothelin); still others remain adhered to the surface of the endothelial cells, carrying out their action by direct contact, as happens for the adhesion molecules for leukocytes or those that affect clotting.
- we must not think of the artery as a simple conduit that guarantees the transport of blood where it is needed. Rather, we must imagine it as a dynamic and complex organ, made up of different cellular and molecular actors
In summary, the endothelium represents the metabolic fulcrum of the vascular wall, to the point of regulating cell proliferation, inflammatory phenomena and thrombotic processes. For this reason, the endothelial tissue plays a critical role in regulating entry, exit and the metabolism of lipoproteins and other agents that can participate in the formation of atherosclerotic lesions.
Stages of formation and growth of atheroma
The process of formation and growth of atheroma, which as we have seen develops over the course of years or even decades, consists of various stages, which we describe below:
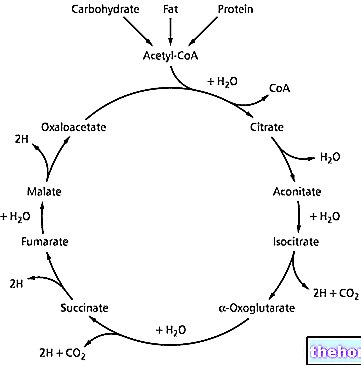
- Adhesion, infiltration and deposition of LDL lipoprotein particles in the intima of the artery; this deposit takes the name of lipid streak ("fatty streak") and is mainly linked to the "excess of LDL lipoproteins (hypercholesterolemia) and / or the defect of HDL lipoproteins. The oxidation of LDL proteins plays a leading role in the processes initial formation of atheroma
- We recall how the oxidation of LDL can be favored by free radicals formed following cigarette smoking (reduced activity of glutathione peroxidase), hypertension (due to an increase in the production of angiotensin II), diabetes mellitus (advanced glycosylation products present in diabetics), genetic alterations and hyperhomocysteinemia; vice versa, the reactive oxygen species are inactivated by dietary antioxidants, such as vitamins C and E, and by cellular enzymes such as glutathione peroxidase
- The inflammatory process triggered by the "entrapment and oxidation of LDL lipids, with consequent endothelial damage, leads to the expression of adhesion molecules on the cell membrane, and to the secretion of biologically active and chemotactic substances (cytokines, growth factors, radicals free), which together favor the recall and subsequent infiltration of leukocytes (white blood cells), with the transformation of monocytes into macrophages;
- we recall how nitric oxide (NO) produced by endothelial cells, in addition to its well-known vasodilating properties, also exhibits local anti-inflammatory properties, limiting the expression of adhesion molecules; for this reason it is currently considered a protective factor against atherosclerosis. Well, physical activity has been shown to increase the synthesis of nitric oxide. In other studies, on the other hand, in response to acute physical exercise, a reduction in endothelial adhesion of leukocytes has been shown, while it has been known for some time that regular exercise is associated with a lower concentration of C reactive protein (thermometer of inflammation) at rest. More generally, physical exercise prevents and corrects certain conditions that pose a risk to atherosclerosis, such as hypertension, hyperglycemia and insulin resistance. In addition, it increases HDL levels and enhances endogenous antioxidant systems, thus preventing the oxidation of LDLs and their deposit in the arteries.
- Macrophages engulf oxidized LDL by accumulating lipids in their cytoplasm and turning into foam cells, rich in cholesterol. Up to this point - while representing a (purely inflammatory) lesion that precedes the atherosclerotic plaques - the lipid streak can dissolve. In fact, only the accumulation of lipids, free or in the form of foamy cells, occurred. In the subsequent phases, the accumulation of fibrotic tissue leads to the irreversible growth of the actual atheroma.
- If the inflammatory response is not able to effectively neutralize or remove harmful agents, it can continue indefinitely and stimulate the migration and proliferation of smooth muscle cells, which migrate from the medial tunic to the intimate, producing extracellular matrix that acts as a structural scaffold of the atherosclerotic plaque (atheroma). If these responses continue further, they can cause a thickening of the arterial wall: the fibrolipid lesion replaces the simple lipid accumulation of the initial stages and becomes irreversible. The vessel, for its part, responds with a process called di compensatory remodeling, trying to remedy the stenosis (shrinkage induced by plaque), gradually dilating in order to keep the lumen of the vessels unaltered.
- The synthesis of inflammatory cytokines by endothelial cells acts as a booster for immunocompetent cells such as T lymphocytes, monocytes and plasma cells, which migrate from the blood and multiply within the lesion. At this point it is believed that as the lesion grows, due to lack of nutrients and hypoxia, smooth muscle cells and macrophages may undergo apoptosis (cell death), with calcium deposition on dead cell residues and on extracellular lipids. This is how complicated atherosclerotic lesions arise.
- The final result is the formation of a more or less large lesion, consisting of a central lipid core (lipid core) wrapped in a fibrous connective cap (fibrous cap), infiltrates of immunocompetent cells and calcium nodules. It is important to underline that in the lesions there may be a great variability in the histology of the formed tissue: some atherosclerotic lesions appear predominantly dense and fibrous, others may contain large quantities of lipids and necrotic residues, while most present combinations and variations of each of these characteristics The distribution of lipids and connective tissue inside the lesions determines their stability, ease of breakage and thrombosis, with the consequent clinical effects.
Watch the video
- Watch the video on youtube
Watch the video
- Watch the video on youtube
Causes
The pathogenesis of atherosclerotic plaques described above demonstrates how atherosclerosis is a complex pathology, the onset of which various components of the vascular, metabolic and immune systems participate.

It is not, therefore, a simple passive accumulation of lipids inside the vascular wall. However, as anticipated, atherosclerotic plaques can occlude the vessel lumen by up to 90% without showing clinically evident signs. The problems are quite serious. , they begin in case of rapid growth of a blood clot (thrombus) following the rupture of the fibrous capsule or the endothelial surface, or to the hemorrhage of the microvessels inside the lesion. Thrombi, formed on the surface or inside the lesion, can cause acute events in two ways:
1) they can enlarge in situ to completely occlude the vessel blocking the blood flow from the point where the plaque develops;
2) they can detach from the lesion site and follow the blood flow until they become blocked in a small caliber vessel branch, preventing the blood supply from that point onwards.
Both of these events prevent the correct oxygenation of the tissues, inducing their necrosis. Vessel occlusion can also be favored by vasospasm induced by the release of endothelin by endothelium cells.
Furthermore, the weakening of the vessel wall can lead to a generalized dilation of the artery, which over the years can lead to the formation of an aneurysm.
To sum up, simplifying the concept as much as possible, the formation of atheromas is the consequence of three processes:
- the accumulation of lipids, mainly free cholesterol and cholesterol esters, in the sub-endothelial space of the arteries;
- the establishment of an inflammatory state with infiltration of lymphocytes and macrophages which, by engulfing the accumulated lipids, become foam cells;
- smooth muscle cell migration and proliferation




.jpg)


















