Generality
When we talk about autoimmune thyroiditis we are not referring to a specific pathology, but to a set of inflammatory diseases on an autoimmune basis that affect the thyroid gland.

Fortunately, autoimmune thyroiditis is a disorder that can be easily treated and controlled, thus allowing patients who suffer from it to live an almost normal life.
Types of Autoimmune Thyroiditis
As mentioned, the term "autoimmune thyroiditis" does not mean a single disease, but multiple pathologies that occur in the thyroid gland.
In truth, to be more precise, in technical terms we prefer to talk about autoimmune chronic lymphocytic thyroiditis, of which there are different forms among which we remember:
- Hashimoto's thyroiditis (also known as Hashimoto's disease);
- Atrophic autoimmune thyroiditis;
- Silent thyroiditis.
Below, the main characteristics of the aforementioned forms will be briefly described.
Hashimoto's thyroiditis
Hashimoto's thyroiditis is certainly one of the best known and most widespread forms of thyroiditis. In fact, more often than not, the term "autoimmune thyroiditis" is used as a synonym for "Hashimoto's thyroiditis".
Usually, the onset of Hashimoto's thyroiditis occurs in a subtle and asymptomatic manner, making early diagnosis difficult. The diagnosis of Hashimoto's thyroiditis is also made even more difficult by the variability of symptoms between patient and patient.
This form of autoimmune thyroiditis is particularly common in women, and its onset is related to genetic risk factors.
In patients suffering from Hashimoto's thyroiditis, the body produces autoantibodies that attack the thyroid gland, to the point of compromising the production of thyroid hormones, thus causing the onset of hypothyroidism.
In response to the reduced levels of thyroid hormones in the blood, the pituitary gland increases the production of the thyroid stimulating hormone (or thyrotropic hormone, better known by the acronym TSH), in an attempt to compensate for the deficiency of circulating thyroid hormones that it has come to be created.
The increase in TSH levels, in turn, causes a compensatory increase in the volume of the thyroid gland itself, culminating in the appearance of the well-known goiter.
Hashimoto's thyroiditis is characterized by the presence in the bloodstream of high levels of TSH and reduced levels of thyroid hormones T3 (triiodothyronine) and T4 (thyroxine).
Atrophic autoimmune thyroiditis
Atrophic autoimmune thyroiditis - similar to what happens with Hashimoto's thyroiditis - can arise subtly and remain asymptomatic for relatively long periods, thus preventing early diagnosis.
Also in this case, atrophic autoimmune thyroiditis manifests itself with the "onset of" hypothyroidism, but without the enlargement of the gland, therefore without the presence of goiter. TSH which hinder the binding of the thyroid hormone to its receptors on the thyroid gland.
Silent thyroiditis
Silent thyroiditis has intermediate characteristics between Hashimoto's thyroiditis (i.e. autoimmune thyroiditis par excellence) and sub-acute thyroiditis (a particular form of thyroiditis that tends to resolve spontaneously or in any case to resolve following a short period of targeted therapy mostly to the resolution of the inflammation).
However, since silent thyroiditis has an autoimmune pathogenesis, it falls within the group of autoimmune thyroiditis.
Like Hashimoto's disease, this inflammatory thyroid disease also occurs with greater incidence in female patients.
The typical clinical manifestations of silent thyroiditis are similar to those of sub-acute thyroiditis (mainly fever and thyrotoxicosis), with the exception of continuous pain in the anterior area of the neck which - contrary to what occurs in sub-acute thyroiditis - is not perceived. by patients suffering from silent thyroiditis. Not surprisingly, this particular form of autoimmune thyroiditis is also defined as "painless" (from the English painless).
Finally, even in this case, anti-thyroid antibodies are present in the bloodstream, although the levels identified are not excessively high.
Diagnosis
The diagnosis of autoimmune thyroiditis is mainly made through the execution of laboratory tests, to evaluate the presence in the blood of anti-thyroid antibodies produced by the immune system and to evaluate thyroid function (determination of the levels of TSH, T3, T4, etc.).
The values thus identified may vary according to the stage in which the autoimmune thyroiditis is found and also change from one patient to another (especially in the case of Hashimoto's thyroiditis).
In addition to laboratory tests, for the diagnosis of autoimmune thyroiditis it is also possible to use radiographic tests, useful for determining the typical inflammation of the thyroid gland that characterizes this type of endocrine pathology.
Symptoms
The symptomatology of the different forms of autoimmune thyroiditis can vary according to the type of disease that has affected the patient and according to the stage in which it is found. Furthermore, the symptoms that occur can be very different even between one patient and another.
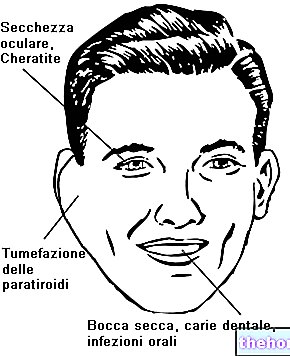
However, among the typical symptoms of Hashimoto's thyroiditis, we remember:
- Weakness and fatigue;
- Drowsiness;
- Pale and cold skin
- Increased sensitivity to cold;
- Constipation;
- Hypercholesterolemia;
- Weight gain mainly due to water retention;
- Increased menstrual flow;
- Hoarse voice;
- Depression;
- Goiter (due to the increase in the volume of the thyroid, caused in turn by the excessive secretion of TSH by the pituitary);
- Myxedema (a complication that occurs in case of severe hypothyroidism not adequately treated).
Among the symptoms that can arise in the case of atrophic thyroiditis, however, we remember:
- Asthenia;
- Dry skin
- Brittle hair
- Increased sensitivity to cold;
- Insomnia;
- Depression;
- Anemia;
- Constipation.
As for silent thyroiditis, on the other hand, patients suffering from this form of autoimmune thyroiditis have symptoms that resemble those that occur in patients with sub-acute thyroiditis. More in detail, among the different manifestations that can occur in the case of silent thyroiditis, we remember fever and thyrotoxicosis (characterized by symptoms such as, for example, tremors, tachycardia and anxiety).
Treatment
Similarly to what has been said for the symptomatological picture, the treatment can also vary according to the form of autoimmune thyroiditis that has affected the patient and according to the stage in which it is when it is diagnosed.
Generally, treatment of Hashimoto's thyroiditis and atrophic thyroiditis aims to restore thyroid function as much as possible. More precisely, this treatment seeks to compensate for the lack of thyroid hormone production through hormone replacement therapy which usually involves the administration of levothyroxine or liothyronine.
As for silent thyroiditis, on the other hand, in most cases hormone replacement therapy is not necessary. However, symptomatic treatment of thyrotoxicosis, which can occur in these cases, may be necessary. In this regard, the drug of choice usually used is the beta-blocker propranolol, an active ingredient that has proved particularly useful in counteracting symptoms such as tachycardia and tremors.
In any case, the type of therapeutic strategy to be undertaken will be established by the endocrinologist on a strictly individual basis, according to the form of autoimmune thyroiditis from which the patient suffers and the stage of the same.